By Dr Minh Alexander retired consultant psychiatrist 11 February 2026
SUMMARY
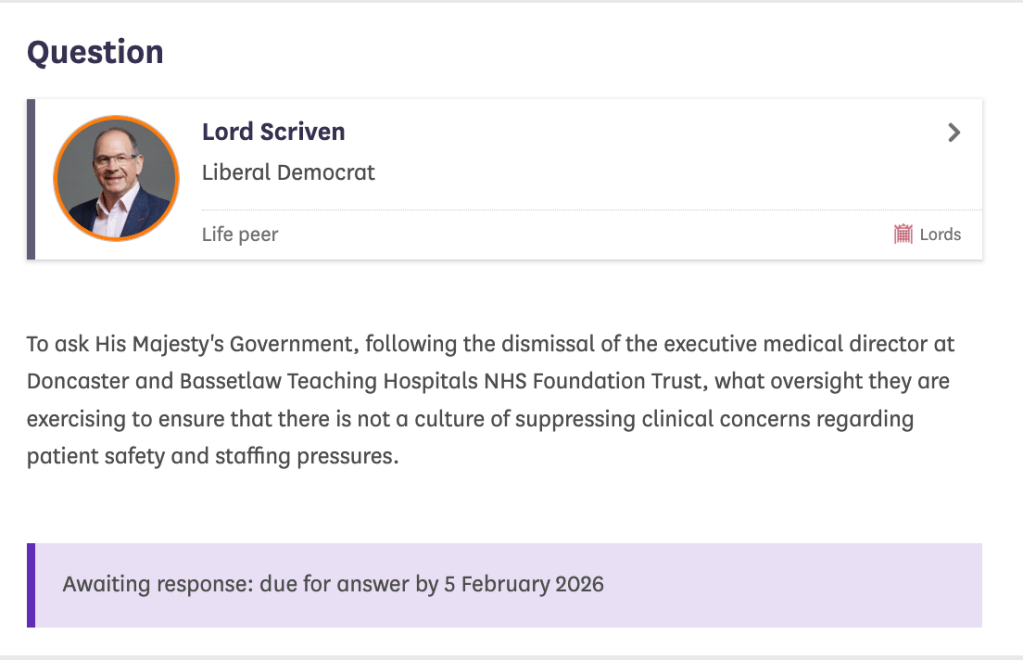
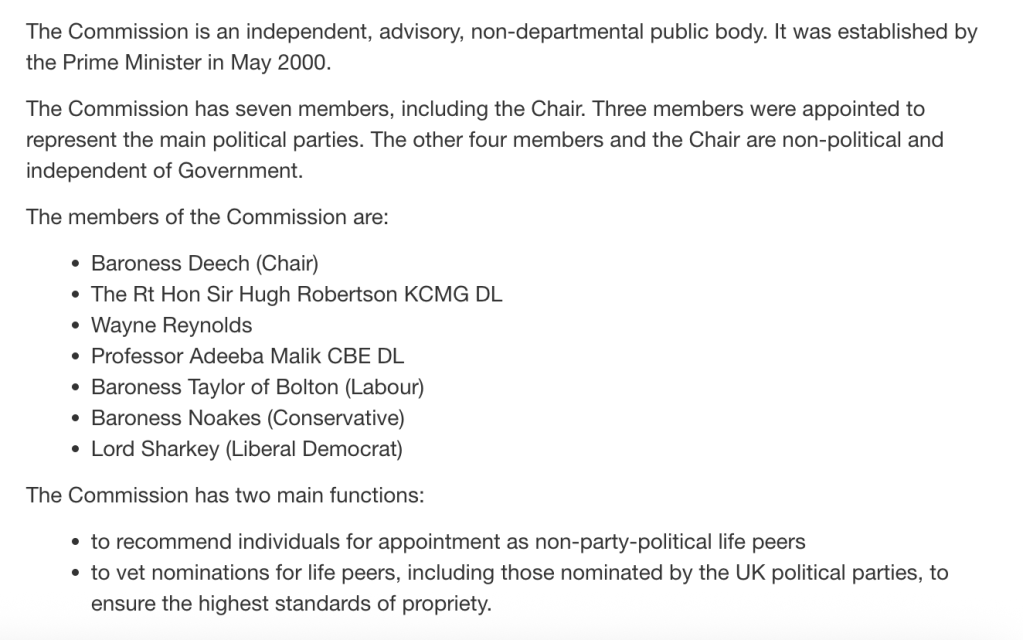
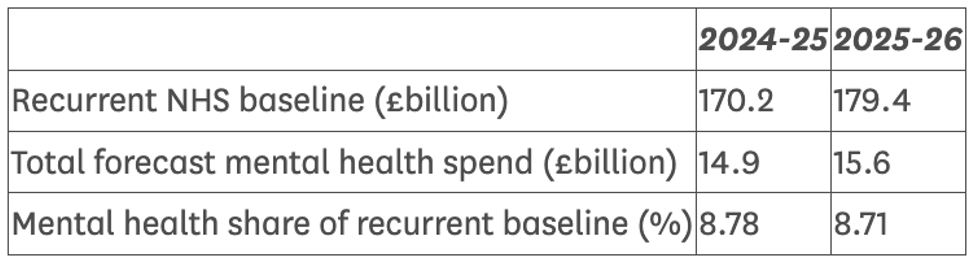
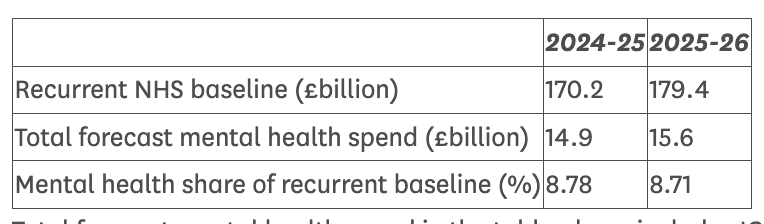
Paul Lipscombe an Associate Director at University Hospitals Coventry and Warwickshire NHS Trust was sentenced on 11 November 2025 to over twenty eight years in prison for extremely serious and sometimes violent sexual offending against female children. He was also sentenced for making and distributing indecent images. A transcript of the sentencing hearing shows that Lipscombe reportedly took “very high risks” in offending, sometimes even whilst taking work conference calls. By Lipscombe’s own report, he had been offending against young girls since his twenties. Sentencing Judge Raynor concluded that Lipscombe was “very highly dangerous”. FOI data shows the trust provided the police with information, but there is otherwise no evidence of meaningful NHS effort, by the trust or the regulator Care Quality Commission, to ensure safe, appropriate learning from these events. There was an alleged agreement, between the trust and the local CQC relationship manager, that Lipscombe’s initial arrest in April 2024 for suspected kidnap of a missing fifteen year old girl was not even a reportable incident. CQC published a brief Well Led inspection report in August 2025, shortly after the trust learnt Lipscombe had pleaded guilty to further offences. CQC concluded that UHCW was “Good” on the Well Led domain. The authors of this report are not disclosed.
INTRODUCTION
Paul Lipscombe was an Associate Director of Performance and Informatics at University Hospitals Coventry and Warwick NHS Trust who was sentenced on 11 November 2025 to over twenty-eight years in jail for a series of extremely serious, calculated sexual offences, including rapes, against female children aged twelve to fifteen. He was also convicted of making and distributing indecent images of children being abused, which related to an online side business that also sold advice to other/would-be sex offenders. The case was widely reported:
NHS manager who groomed young girls on Snapchat jailed for 28 years for rape and abuse
Lipscombe pleaded guilty to a total of 34 offences, but was criticised by the judge for not admitting guilt at an early enough stage.
The full extent of Lipscombe’s crimes is uncertain. Healthcare Management Magazine noted after his sentencing that: “A police investigation into the scale of Liscombe’s crimes continues.” The police portal for that investigation can be found here.
Reflecting the seriousness of his offending, Lipscombe’s sentence consists of a three year sentence which is to run consecutively with a twenty five year sentence. He is not eligible to apply for parole until two thirds of the twenty five year sentence has been served. He was 51 at the time of sentencing and so at the earliest will not be on licence until 70.
To put Lipscombe’s heavy sentence in context, the average sentence for child sex abuse between 2015 to 2019 was three years and four months. In 2019, only 124 people received sentences of more than twenty years (across all offence types), barring life sentences. In 2021, the Prison Reform Trust reported that there were a total of only 894 people across the prison estate who were serving determinate sentences of 20 years or longer.
Lipscombe was given an Extended sentence under section 280 of the Sentencing Act 2020, relating to rape of a child under age 13. In 2024, only 1200 people received extended sentences.
The police described Lipscombe’s crimes as “horrendous” and indicated that they were some of the most serious sex offences they had handled.
A summary of the police investigation and a helpful list of the specific offences can be found here.
Lipscombe’s case clearly raised issues of NHS managerial Fit and Proper Persons.
His former employing trust released a deflective statement, which emphasised that Lipscombe had an “administrative” and not a “patient facing” role.
UHCW also claimed to have carried out its “own internal review” and that “nothing has been identified at this stage to indicate this individual’s criminal activity was committed as part of their role”.
| [UHCW] “Statement in relation to the sentencing of former employee, Paul Lipscombe 11 November 2025 We would like to praise the girls and their families, as well as Leicestershire Police, for their bravery and courage in bringing Paul Lipscombe to justice for his horrendous crimes. Following Lipscombe’s arrest in April 2024, we immediately suspended him before dismissing him from his administrative, non-patient facing role in June 2024. The Trust has and will continue to support Leicestershire Police with its investigations and has carried out its own internal review – nothing has been identified at this stage to indicate this individual’s criminal activity was committed as part of their role. For anyone who would like to report information or possible offences committed by Lipscombe, visit: Public Portal You can also call Leicestershire Police on 101. In an emergency always call 999. For more information around spotting the signs of grooming and where to get further support, visit: https://www.leics.police.uk/advice/advice-and-information/gr/grooming/ |
JUDGE’S SENTENCING REMARKS
In an attempt to get a better sense of the case details, and especially the length of offending and potential relevance of Lipscombe’s offending to his NHS employment, I asked the Court for a transcript of the sentencing remarks.
Because of the extremely unpleasant material about Lipscombe’s offending therein, I am not posting the transcript.
I instead summarise and provide the most salient excerpts for the purposes of this post.
But the whole document is available as verification, if required.
It is clear from the sentencing hearing that Lipscombe was an entirely unsuitable person to be responsible for healthcare services, responsible for vulnerable people and/or people at vulnerable times in their lives, or responsible for overseeing staff and their welfare.
His offending was cold, intentionally degrading, manipulative and at times coercive and violent. At times he hurt his victims, and said that he intended to do so.
The Probation Officer who prepared the pre-sentence report concluded that the offences were planned and featured pre-meditation.
Lipscombe was controlling of victims and he engineered damaging attachments with victims to facilitate the sexual offences.
The defence attributed these attachments in part to victims’ pre-existing vulnerabilities:
“He developed, with a very small “r”, relationships with the girls, and it is right and fair to say that the girls, because of the level of grooming, and because of their vulnerabilities, believed at the relevant time that they were in such relationships with him.”
Another view is that offenders target the vulnerable.
In return for payment, Lipscombe also tutored other predators in his grooming methods. The minutely calculated nature of his grooming and manipulation of children is vividly illustrated in these communications.
The tone in these communications is one of pride and satisfaction in his achievements, by his own lights. In one communication, Lipscombe stated that the information he was selling was worth far more than the fee charged. In Lipscombe’s comments, victims are objectified, their feelings considered in so far as manipulation was a means to facilitating offending.
Victims’ privacy was violated by Lipscombe’s secret recordings, and the Court noted from the Probation pre-sentence report that images may still be circulating on the internet:
“…in some instances they were secretly recorded, thus violating privacy, and any images shared online may remain there permanently, and not be totally removed.”
Lipscombe was married and the Court noted that he also misled his wife, telling her that he was away on work trips when he was pursuing victims:
“…you lived in a nice house with your wife, and were proud of your wealth and the Tesla car parked up on your drive. You told your wive [sic], for instance, that you were going on business trips to London, but in truth you were travelling to engage in your obsession, namely sexually abusing young girls.”
According to the media, the prosecution also held that Lipscombe tried to blame others:
“He [Lipscombe] accused other people of serious crimes simply in order to mask his own crimes”
At sentencing, Judge Keith Raynor praised the thoroughness of the pre-sentence Probation report, which noted that even when on remand, Lipscombe wrote sexualised stories, which echoed elements of his own offending. He handed these stories to prison educational staff. Judge Raynor concluded from this behaviour that the sexual offending was “engrained” in Lipscombe.
Judge Raynor noted inconsistent expressions of remorse and that the pre-sentence Probation report had described victim-blaming by Lipscombe.
“When we deal with the question of remorse, he has expressed some remorse to a psychiatrist. To the pre-sentence report author he has victim blamed, and he has said that these offences in part occurred because the victims were promiscuous. That is not indicative, it seems to me, of anyone with genuine remorse.”
At the conclusion of proceedings, Judge Raynor noted a letter of apology by Lipscombe and decided: “In the circumstances I have decided to give him a morsel in respect of remorse.”
It is notable that Lipscombe’s defence barrister cited his NHS service as a factor in mitigation.
“So far as these matters are concerned, your Honour is dealing with a 51-year-old man. He has no criminal convictions before this date. He was also an award winning employee at the National Health Service because of the work he had done, particularly during covid, in reducing waiting times for patients, and in improving the computer systems, those are facts.
He did live, aside from this awful part of him, a good and decent life, and was a useful member of society. He did all of that whilst having ADHD and autism, and he continued to work.”
The defence also pointed to reported psychiatric factors of ADHD and “autism”. However, Lipscombe’s behaviours suggest high social functioning that may not be entirely consistent with the latter.
Judge Raynor noted that the pre-sentence Probation report described “sophisticated predatory behaviour”.
Indeed, the sentencing hearing also revealed that Lipscombe had obtained a position of responsibility and sensitivity in custody as a “Listener”, about which the reporting Probation officer had expressed some concern. Listeners in theory act as confidential emotional supports to other prisoners, who may be in crisis and or suicidal, and therefore a level of social function is needed.
In weighing the case at sentencing, Judge Raynor identified the following aggravating factors:
“manipulation”
“deviousness”
“controlling and obsessive behaviour”
“committing offences in a victim’s home”
“Telling L it had to be a secret”
“The distances you travelled to engage in your sexual activity”
“The fact that there was ejaculation”
“The spy camera 54-minute video”
“The upskirting”
“The grooming”
“The snapping of the Sim and the factory reset with S”
“The disparity of age”
“On occasions force being used”
“child known to the offender”
“severe psychological harm”
“Additional degradation, humiliation”
“Violence or threats of violence”
“Forced uninvited entry into a victim’s home”
“a child being particularly vulnerable due to personal circumstances”
“moving images”
“active involvement in a network which facilitates the sharing of images”
“profiting from the distribution”
Judge Raynor concluded that Lipscombe was “very highly dangerous”:
“The dangerousness of you, it shouts out from the evidence in this case, it then becomes utterly compounded by the contents of the pre-sentence report, and I have a firm view that you are very highly dangerous”
Importantly, Judge Raynor also noted that Lipscombe took “very high risks” in his offending:
“You were bold in your offending, and you took very high risks, which I am sure made things more exciting for you. You committed offences in your own home, at the same time as working from home and taking conference calls. You also sexually assaulted one victim in her own house.”
This raises questions about the degree to which there may have been signs during Lipscombe’s offending that others could have acted upon, to help stop him.
Also very importantly, during the preparation of the pre-sentence Probation report, Lipscombe reportedly disclosed that he had been offending against girls since he was in his twenties:
“…he has been committing sexual offending against young girls since he was in his 20s”
That is to say, it is possible that Lipscombe was offending through much or all of his NHS career.
This Probation evidence was supported by online chat data recovered by the police, in which Lipscombe informed another male of very longstanding sexual urges towards children.
It is of course possible that Lipscombe was so skilful in his deceptions that he functioned “normally” at work, at a superficial level, and that the NHS cannot be fairly criticised for not detecting any abnormality or risk to others.
And it is of course easy to criticise in hindsight.
But after such a catastrophe, it would be good practice to reflect and ensure organisational learning where relevant.
Moreover, systems weaknesses may be spotted upon review, even when there have not been failings.
UNIVERSITY HOSPITALS OF COVENTRY AND WARWICKSHIRE NHS FOUNDATION TRUST’S RESPONSE
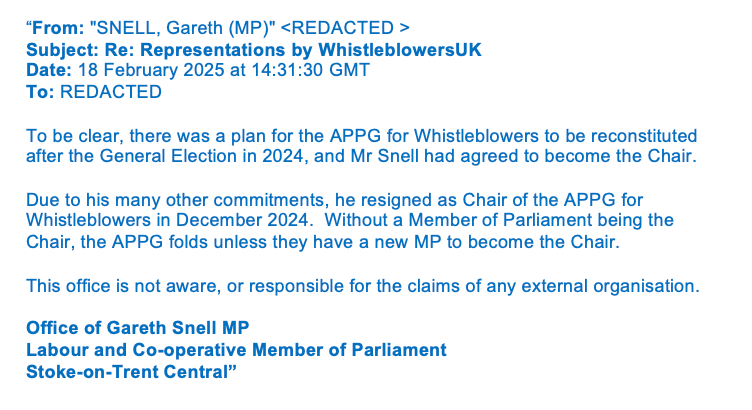
I asked the trust about its internal response to Lipscombe’s case. Two FOI requests, and a note to the trust informing it that I had made referral to the ICO, were needed to elicit reasonable information. The trust appeared reluctant to answer supplementary questions which probed further, and it delayed in responding to the second FOI request.
It appears that despite the trust’s claim that it undertook “an internal review”, there was no meaningful learning exercise.
The trust admitted that it only checked devices and for evidence of any inappropriate access to patient information by Lipscombe as part of the police investigation.
“In liaison with the police, the Trust reviewed whether there was any evidence that PL had used any Trust devices to make contact with children and whether there was any inappropriate material on any of his Trust devices. The Trust also reviewed whether there was any evidence that PL had made any inappropriate access to patient information as part of his non patient contact role.”
There was no evidence that the trust fully considered its governance, human resources practice, possible failures to spot signs of a serious offender or the impact on colleagues of working with Lipscombe. In particular, the experience of female subordinates would have been important to review, one would have thought.
Moreover, the directors in charge of the trust’s response to the police were the Chief People Officer (Donna Griffiths) and Director of Performance & Informatics (Dan Hayes), who both arguably had conflicts of interest in the matter. This is because Lipscombe was an associate director in Performance and Informatics and his offending also raised questions about trust HR practice.
“The review was undertaken by the Director of Performance & Informatics, Director of ICT & Digital and Director of Workforce reporting to the Chief People Officer on behalf of the Trust Board”
In its first FOI response to me, the trust answered misleadingly when asked if it had checked processes for ensuring the fitness of its managers, especially directors, and whether there were Safeguarding issues arising from Lipscombe’s employment at the trust. It replied:
“There was no failings identified as part of the support to the criminal investigation or in relation to Trust processes”
when the scope of the trust’s actual response could not have answered or fully answered either of these questions.
The trust was more careful when asked if there has been evidence of other employees acting in concert with Lipscombe, and gave the following reply:
“As confirmed in our press statement we supported and continue to support the police in their criminal investigation. No concerns have been reported to the Trust and we continue to support their investigation.”
UHCW admitted that there had been three other cases in the last five years of alleged sexual offending by other trust employees, but maintained these were unrelated to the Lipscombe case.
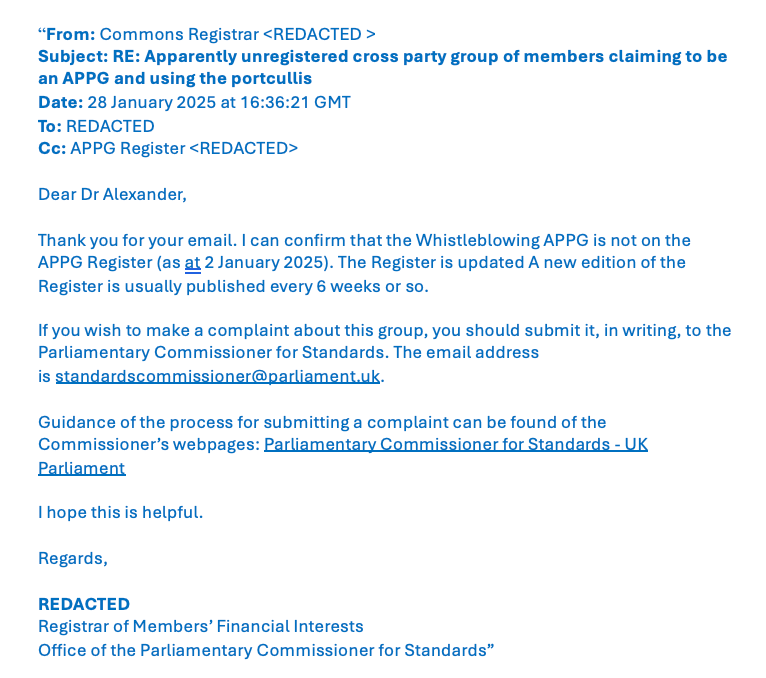
UCWH revealed that it did not formally inform the regulator the Care Quality Commission (CQC) of Lipscombe’s arrest in April 2024, and only informed CQC about Lipscombe in August 2025.
On further questioning, UHCW claimed that the initial arrest in April 2024 did not trigger CQC reporting requirements and that the local CQC relationship manager agreed with this view:
“On 23rd April 2024, the Trust was informed that PL had been arrested for a serious criminal charge involving one person. The Trust made an initial assessment that the CQC would not need to be informed. A verbal conversation with the CQC relationship manager confirmed that the incident did not trigger Regulation 18.”
See here for information on CQC Regulation 18, which relates to staffing requirements. It is arguable that other CQC regulations were also relevant.
Interestingly though, UHCW indicated that it informed NHS England of events in June 2024, so there was recognition that Lipscombe’s arrest was a significant matter.
“The Trust also informed NHSE of this matter on 5th June 2024.”
I fail to see how the arrest of a senior NHS manager on a “serious criminal charge” (the trust’s words) is not reportable to the CQC and should not trigger a review of Fit and Proper Persons CQC Regulation 5 or other potentially relevant CQC Regulations, regardless of whether the offending is against one person or several people. The original arrest in April 2024 was for suspected kidnapping of a missing fifteen year old girl. If neither UHCW and CQC consider this a reportable matter, what hope is there? Moreover, after the police found the missing girl with Lipscombe and took her to a place of safety, she reportedly disclosed that he had raped her. Were UHCW and the CQC were aware of this?
The events above, as reported by UHCW, raise not only questions about the trust but also about the local CQC relationship manager.
The trust claims it was notified on 6 August 2025 that Lipscombe pleaded guilty to additional charges, and at that point it formally reported to CQC:
“On 6th August 2025, the Trust was informed that PL’s court case was due to commence in late August 2025 and that PL had pleaded guilty to further criminal charges. The CQC were formally notified on 6 August 2025.”
For accuracy, the police summary states that Lipscombe in fact pleaded guilty to the 34 offences in February 2025.
These are the two FOI responses by UHCW:
Paul Lipscombe UHCW FOI response 22 December 2025
Paul Lipscombe UHCW FOI response 10 February 2026
CQC’S RESPONSE
It is notable that only nine days after formal notification by UHCW of Lipscombe’s guilty plea to additional charges, the CQC conducted a Well Led assessment of UHCW on 15 August 2025. CQC somewhat dubiously concluded that the trust merited a rating of “Good”.
There is no indication by CQC in its report of why a Well Led assessment was triggered, and no reference to the fact that a senior trust employee was being prosecuted for multiple serious offences, or to the trust’s governance response to this. CQC concluded that the trust was compliant with the Fit and Proper Persons’s requirements. “The trust followed the NHS England guidance for ensuring those persons who met the criteria in Regulation 5 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014 were fit and proper to carry out their roles.” This relates mainly to administrative processes.
The report of the CQC inspection was brief and directly published on CQC’s UHCW webpage, without details of the inspection team who had conducted the inspection. Was it led by the same CQC relationship manager who had failed to act when informed of Lipscombe’s arrest in 2024?
It is remarkable that there was silence about major criminality by a senior trust manager when CQC knew by that point that Lipscombe had pleaded guilty to so many serious offences. It is, as the police said, a horrendous case.
I will raise these various matters with CQC.
So, as Lipscombe embarks on his long prison sentence and drifts from public view, the NHS waters close over with barely a ripple.
It may be that there would not have been a great deal to learn, had a properly accountable and diligent learning process been launched.
But we will probably never know, will we?
RELATED ITEMS
Not many may be aware, but Carl Beech the notorious sex offender and source of bizarre, malicious allegations about a VIP sex ring was, incredibly, a CQC inspector.
He was imprisoned for his crimes in 2019, having been sentenced to eighteen years in prison, but released early last week.
The victims of his malicious allegations were reportedly given no warning of this.
Carl Beech, CQC inspector, convicted child sex offender and fraudster: Activities at the CQC
The CQC informed me that it reviewed potential risks that Beech posed in his duties as a CQC inspector:
“…we have reviewed all records to identify any risks from the inspections and CQC activities that he was involved in and we have no information of concern about his conduct on any inspection. All of the providers have been notified of his involvement in the inspection of their services.”
Perhaps CQC should have applied similar expectations to UHCW’s response to Lipscombe’s offending.
Lipscombe’s victims’ and victims’ families’ statements published by Leicestershire police can be found here. Some of the victim impact evidence was also discussed towards the end of the sentencing hearing. Serious psychiatric injury and ongoing suffering, unsurprisingly, were reported.
Letter to Dr Arun Chopra CQC Interim Chief Executive 12 February 2026