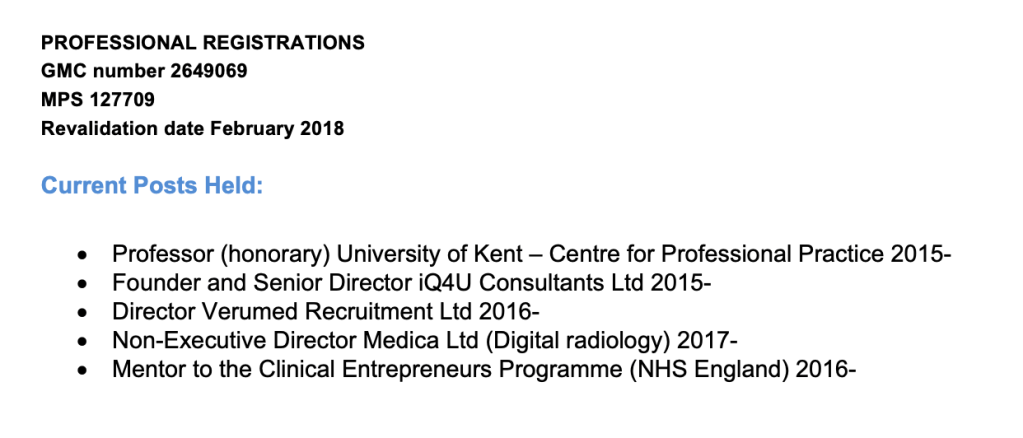
By Dr Minh Alexander retired consultant psychiatrist 6 April 2023
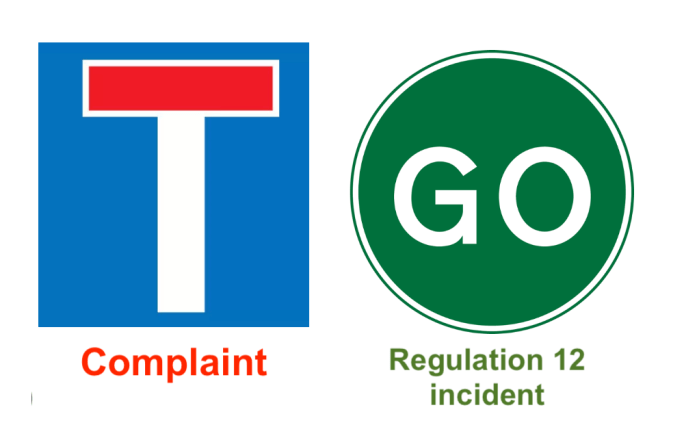
Summary: CQC has once more given scant regard to Employment Tribunal findings of gross whistleblower reprisal in the case of Dr Ambreen Malik and found a provider organisation, Cygnet Health Care, compliant under CQC Regulation 5 Fit and Proper Persons. CQC continues to make claims that it cannot make judgments about the fitness of individuals, and makes unsustainable regulatory judgments about process without taking into account the character of individuals of concern. CQC steadfastly and disingenuously claims that it has no remit to assess the fitness of individuals, despite Regulation 5 requiring that directors are of “good character”. It is also despite the fact that CQC’s own internal guidance states clearly that CQC has powers to take action against providers who have unfit directors, which of course is predicated on CQC making an assessment of individual fitness. CQC also provides almost no details about how it reaches its FPPR decisions, conveniently making them much harder to challenge.
Introduction and background
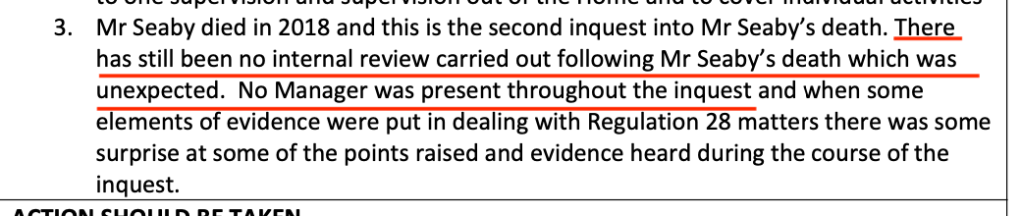
Two years ago I referred Cygnet directors who had been seriously criticised for harming a whistleblower to the Care Quality Commission under CQC Regulation 5 Fit and Proper Persons (FPPR).
Under this regulation, the CQC has powers to ensure that a provider has satisfactory processes for ensuring that its directors are Fit and Proper Persons.
The CQC has typically manipulated matters to allow board members of regulated bodies to evade accountability for serious wrongdoing.
It has done so by claiming that it has no remit to assess if individual directors are Fit and Proper Persons.
Instead, CQC claims it can only look at processes.
This is of course arrant nonsense. If for example, a regulated organisation appoints a freshly convicted serial killer to its board, even CQC might be forced to admit that based on an assessment of the individual, the provider was in breach of FPPR.
CQC Regulation 5 demands that directors must be of “good character”:
- “The requirements referred to in paragraph (2) are that—
- the individual is of good character,
- the individual has the qualifications, competence, skills and experience which are necessary for the relevant office or position or the work for which they are employed,
- the individual is able by reason of their health, after reasonable adjustments are made, of properly performing tasks which are intrinsic to the office or position for which they are appointed or to the work for which they are employed,
- the individual has not been responsible for, been privy to, contributed to or facilitated any serious misconduct or mismanagement (whether unlawful or not) in the course of carrying on a regulated activity or providing a service elsewhere which, if provided in England, would be a regulated activity, and
- none of the grounds of unfitness specified in Part 1 of Schedule 4 apply to the individual.”
Moreover, CQC’s own internal guidance shows that CQC is perfectly aware that it can use other regulations to force the removal of unsuitable provider directors, should it wish to.
“It is not the responsibility of CQC to ensure fitness although we can take action against the provider if we believe an unfit person to be in a directorship position.”
That is the key issue. Does CQC wish to?
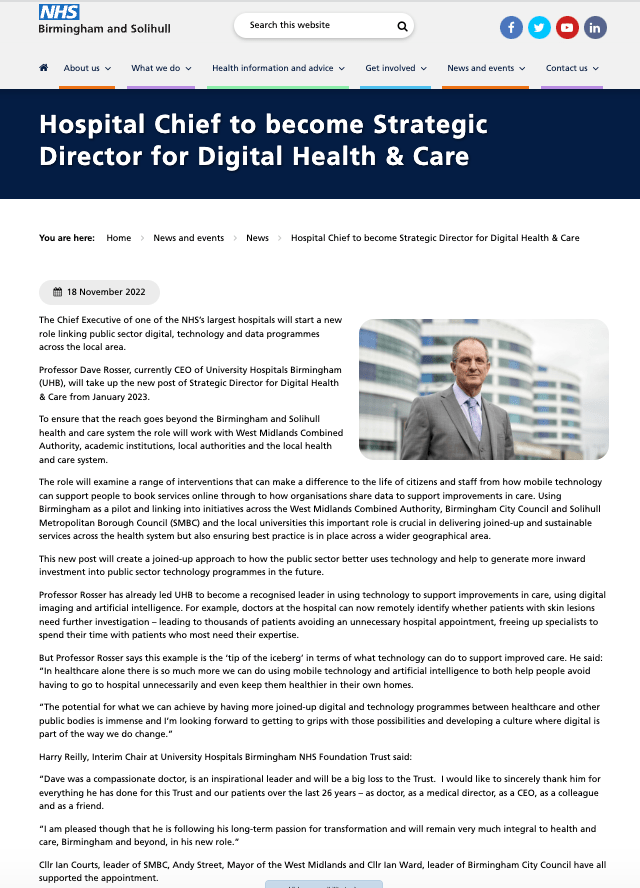
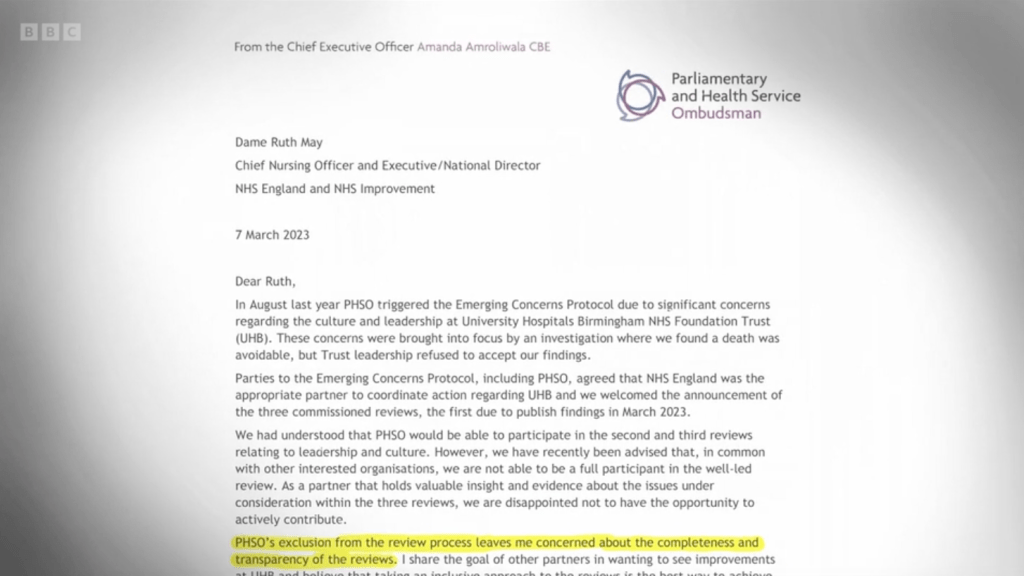
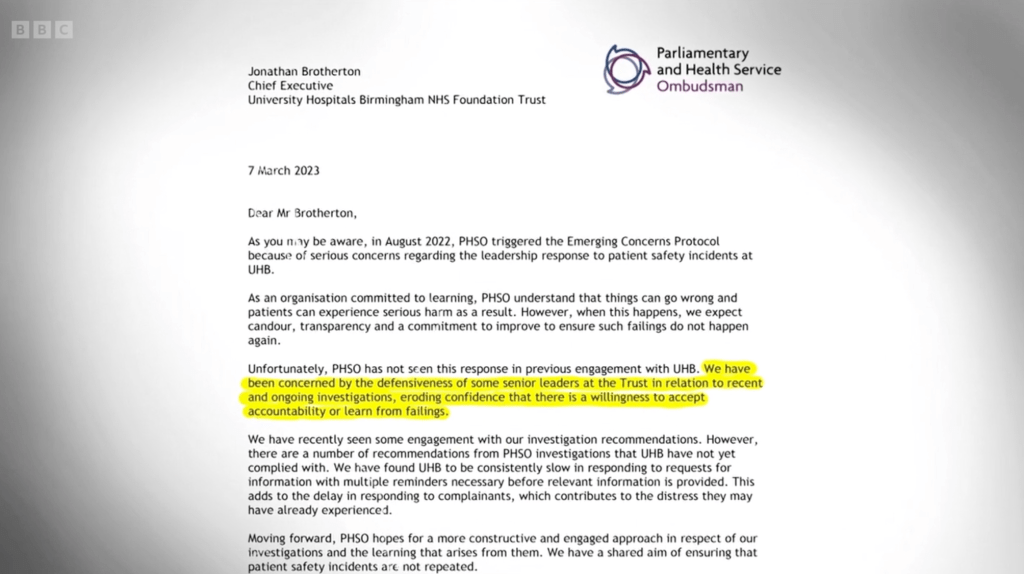
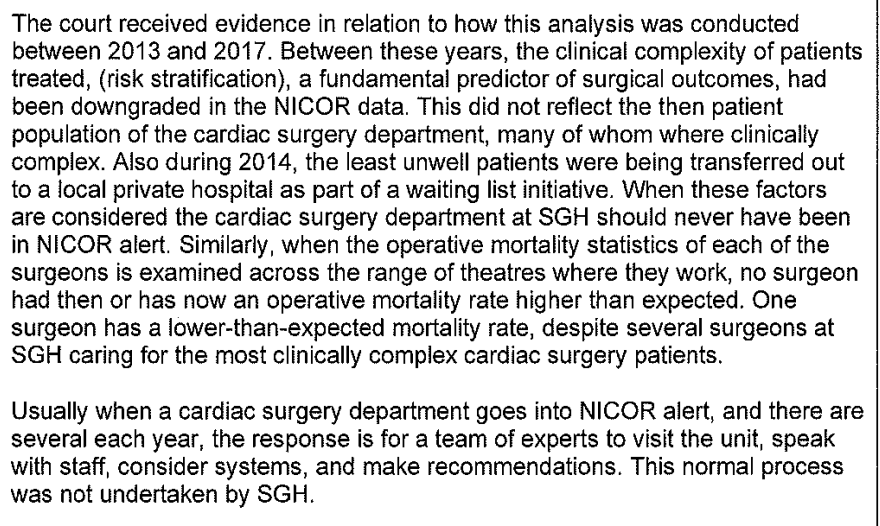
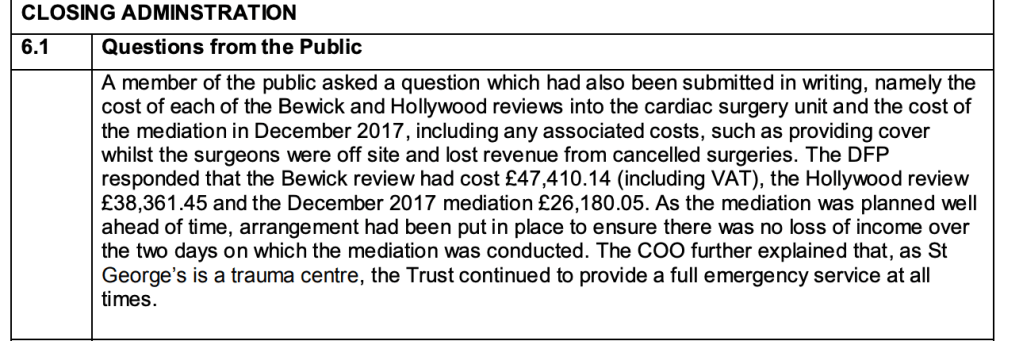
Current media interest in CQC’s handling of FPPR and the UHB scandal
CQC’s disgraceful handling of FPPR is back in the full glare of publicity because the controversial investigator for the UHB scandal Mike Bewick has omitted to examine UHB’s much-criticised FPPR process in his phase one review of UHB.
This has provoked criticism from an external reference group which includes local politicians, who have questioned whether there has been a cover up at UHB:
“There are also several gaps in the report including the lack of recommendation resulting from the conflicting CQC reports. We must be granted access to previous documents such as the Fit and Proper Person Review (FPPR) which have not been shared. Releasing these reports and details of the process and people involved in commissioning and carrying them out is important to help ascertain any conflicts of interest, whether decisions made have contributed to the propagation of UHB’s toxic culture, and whether these amount to a ‘cover up’
Bewick’s omission of FPPR issues from his review relied on a false premise.
Bewick claimed that he did not request a copy of UHB’s still secret FPPR investigation or investigate UHB’s handling of FPPR because it was not within the scope he had been given:
This was peculiar because the terms of reference given to Bewick allowed him to go wherever the evidence took him:
“The review will be independent and without limits but will include….”
Opening the can of FPPR worms at UHB would have involved exposing the CQC’s wrongdoing on FPPR at UHB as well.
Unsurprisingly, Bewick kicked that can down the road.
In this political backdrop, another astonishing but fully predictable CQC failure on FPPR has concluded in the whistleblowing case of Dr Ambreen Malik at Cygnet Health Care.
CQC’s contention that Cygnet is compliant with FPPR
After I referred the relevant Cygnet directors to CQC under FPPR in the light of the extremely critical judgment against Cygnet for whistleblower reprisal, the CQC delayed and justified the delay because Cygnet had appealed against the ET.
During this time, thousands of Cygnet patients remained potentially exposed.
Only after lengthy legal proceedings concluded did CQC wrap up the FPPR process.
If CQC was concerned about patients, it would have independently reviewed Cygnet’s compliance with Regulation 5 without delay, and taken the approach that it would update any assessment if new information emerged.
In the UHB matter, CQC found UHB compliant with Regulation 5 but added that it would “reserve the right to review the case if further information is presented to the CQC”.
When it suits, in the pursuit of protecting the powerful, the arbitrary CQC will do as it pleases.
Notwithstanding, long after the original FPPR referral and with much, much suffering by Dr Ambreen Malik in between, CQC eventually wrote to me on 20 March 2023 with its standard, high handed FPPR closure letter.
The letter came from CQC’s latest Chief Inspector of Hospitals, Sean O’Kelly, and ended with the signature CQC equivalent of shutting the door in a correspondent’s face:
“This concludes CQC’s review of Cygnet Health Care under this regulation, as well as our correspondence with you on the application of Regulation 5 to all information you supplied.”
For the sake of Dr Malik’s privacy I am not going into details, but the shocking disparity between CQC’s inaction and indifference, and everything that she has suffered is truly unforgivable.
Also, with impeccable timing CQC chose to shut down this Cygnet FPPR in the middle of the five week criminal trial of staff from Whorlton Hall (a Cygnet facility) , regarding abuse against highly vulnerable residents. This abuse was enabled by CQC’s failures to act upon the concerns of its own staff, including CQC whistleblower Barry Stanley Wilkinson.
The nine defendants in the Whorlton Hall abuse trial:

I questioned the lack of information provided on CQC’s FPPR decision, citing CQC’s proven and serious unreliability in the Rosser FPPR referral.
This was met with slightly more information on 3 April 2023, including a disclosure that O’Kelly is the current Chair of CQC’s FPPR committee, which makes the decisions on referrals:
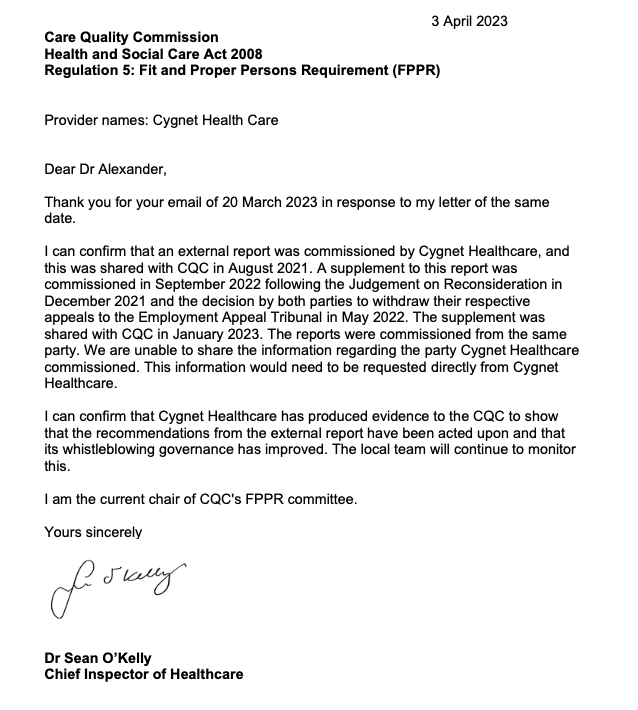
O’Kelly’s role as chair of CQC’s FPPR committee introduces a potential conflict of interest. He may be faced with FPPR referrals which challenge the validity of previous, favourable CQC ratings for which he has ultimate responsibility as Chief Inspector.
Laughably and cynically, CQC suggested that I should contact Cygnet for a copy of the reports upon which CQC’s exoneration of Cygnet was based.
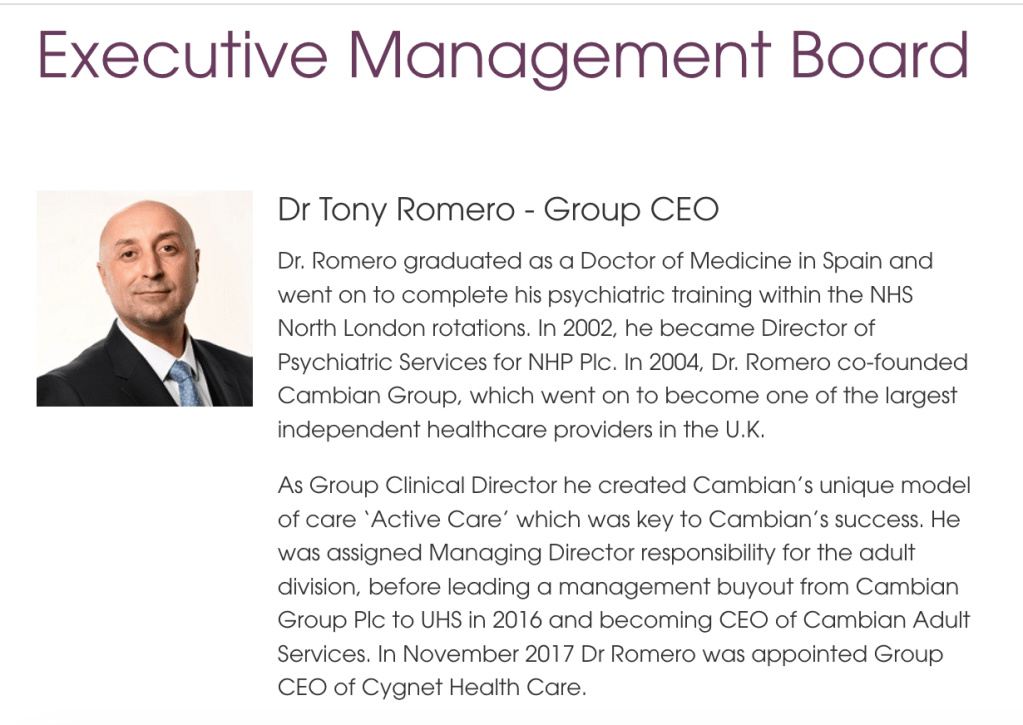
But for completeness, I will ask for a copy from Tony Romero Group CEO of Cygnet Health Care, whom the original ET criticised.
I doubt that Cygnet would be likely to willingly disclose their reports.
And of course, Cygnet Health Care is a private provider and beyond the reach of FOIA, so the reports cannot be obtained by this route either.
CQC’s ridiculous contention that Cygnet is compliant with FPPR because Cygnet’s whistleblowing processes have purportedly improved is predicated on an assumption that individuals change.
Some individuals are not capable of and may not wish to change. No amount of improved processes will protect patients or whistleblowers from such individuals.
That is why less compromised regulators actually ban failed/ rogue directors.
For example, Neil Cruickshank the former senior manager ultimately responsible for the Winterbourne View abuse scandal, who did not listen to whistleblowers’ disclosures, was banned for eight years by the Insolvency Service.
It is a pity that the same cannot be done to CQC, who failed to listen to the Winterbourne View whistleblowers and still fail horribly to listen to or protect whistleblowers by removing abusers.
I also asked NHS England on how it could exert its commissioning leverage to improve whistleblowing governance in the private sector. I have had no response despite numerous chasers.
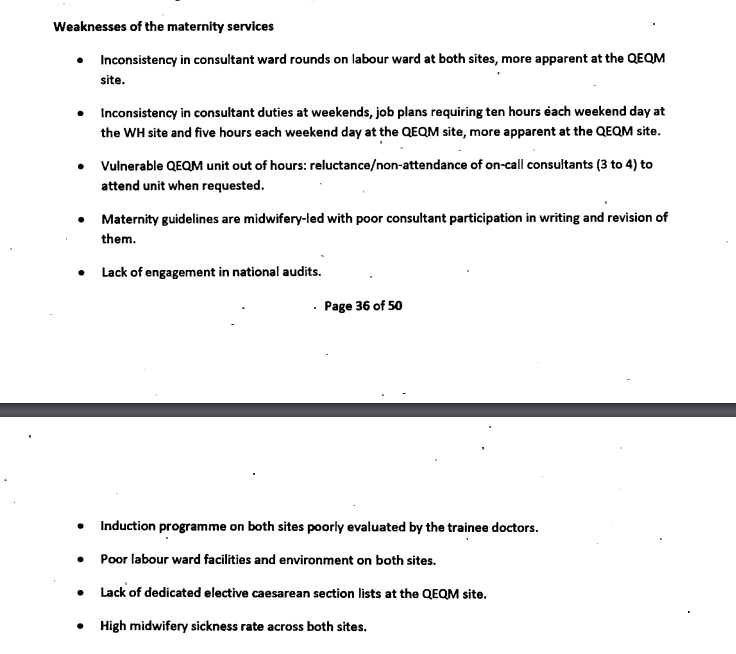
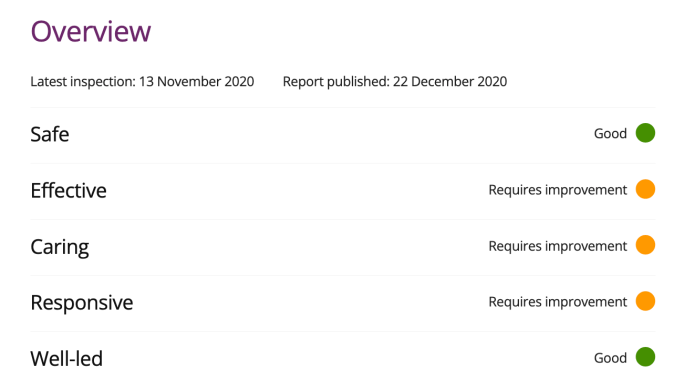
It is also moot whether processes at Cygnet have genuinely improved. Scandals continue to emerge on a regular basis about Cygnet facilities, and most seriously of all, some of the scandals feature lack of learning and improvement after previous identification of failings.
Questions remain
Are some providers too big, wealthy and powerful to be allowed to fail?
And what of the revolving door between regulators and such powerful providers?
How many senior managers in our regulators have their eyes on the glittering prizes on the other side of the fence, and does that affect how they discharge their regulatory duties?
Sir David Behan appointed chair of HC-One
Loss-making care home firm HC-One, pays £1.8m dividend to its private equity owners
UPDATE
I have written as planned to asked Cygnet for a copy of their external FPPR reports:
BY EMAIL
Dr Tony Romero
CEO Cygnet Health Care Ltd
6 April 2023
Dear Dr Romero,
External FPPR reports
The Care Quality Commission has informed me that an Fit and Proper Person referral that I made on Cygnet directors under CQC Regulation 5 in 2021 has concluded, with the regulator concluding that whistleblowing processes at Cygnet have improved to the point where CQC considers that Cygnet is now meeting the requirements of Regulation 5.
I asked the CQC if there had been any transparency about the findings of external reports commissioned by Cygnet which the CQC relied upon to reach its conclusion of improvement.
The CQC did not reply directly to this question but suggested that I contacted Cygnet if I wanted copies of these external reports. They are:
– The external report shared with CQC in August 2021
– A supplement to this report in September 2022, which was shared with CQC in January 2023
In the NHS, the best practice guidance from NHS Providers is that there should be transparency about FPPR investigation findings, at least in summary form.
NHS Providers’ guidance also emphasises that visible rigour is important in contentious cases and where there have been failures of whistleblowing governance.
I would be grateful if Cygnet could accordingly disclose either copies of the external FPPR reports that it commissioned, or at least a summary of the main findings and recommendations.
I copy this to Sean O’Kelly CQC Chief Inspector of Hospitals, Amanda Pritchard CEO of NHS England in view of commissioning issues, and the relevant House of Commons committees.
Many thanks.
With best wishes,
Minh
Dr Minh Alexander
cc Sean O’Kelly CQC Chief Inspector of Hospitals
Amanda Pritchard CEO NHS England
Health and Social Care Committee
Joint Committee on Human Rights
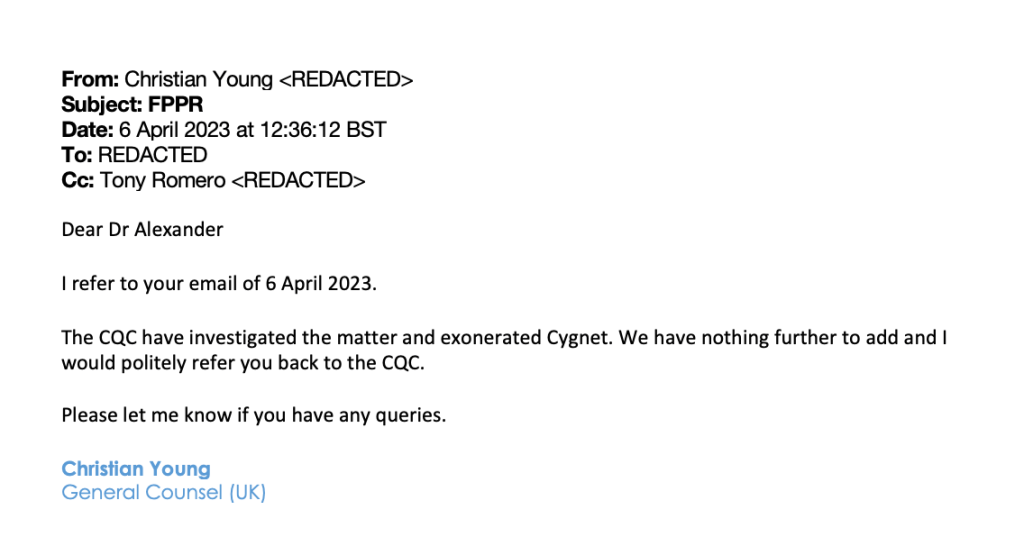
I sent the above request to Cygnet on 6 April 2023 at 11.55 am.
I received the following reply from Cygnet’s General Counsel at 12.36 pm.
RELATED ITEMS
Joint Committee on Human Rights: False reassurance serves only to perpetuate abuse & shield abusers
CQC Whorlton Hall Cover Up: More CQC responses & culpability
Counting the cost of the CQC: Abuse, Whorlton Hall and CQC spin doctors
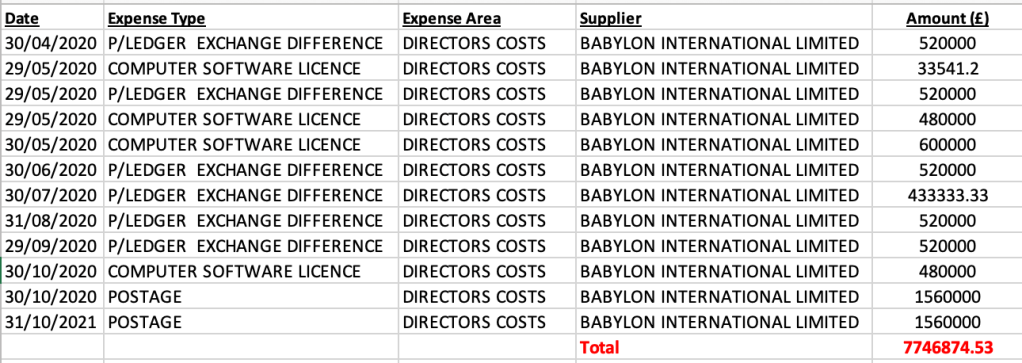
NHSE, ICB and UHB’s three-ring circus and Rosser’s digital assignment
Sorry is the hardest word: CQC, Paula Vasco-Knight and Regulation 5 Fit and Proper Persons