Dr Minh Alexander retired consultant psychiatrist 6 July 2023
Disappointing BBC News coverage featured Robert Francis and the latest NHS Freedom To Speak Up Guardian Jayne Chidgey Clark on 3 July 2023.
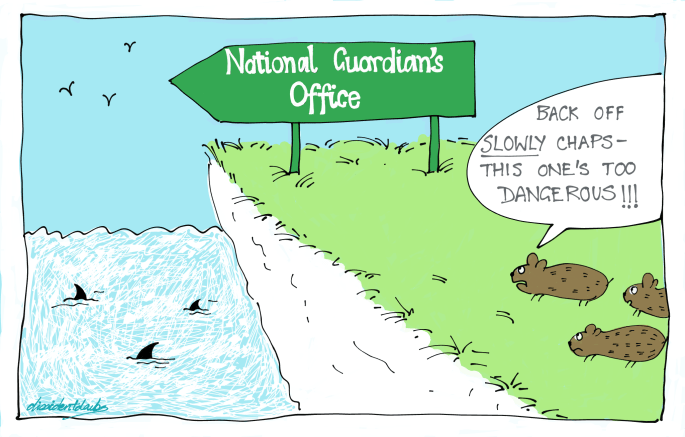
The piece helped to legitimise the National Guardian’s Office, when it is in fact a threat to NHS whistleblowers.
The BBC team who produced the material did not balance claims by the National Guardian with evidence of her Office’s failures or with criticisms of her Office by whistleblowers.
They also chose not to include whistleblowers with the strongest cases which exposed the serious failings of the National Guardian’s Office. Whistleblowers from whom they had agreed to take this evidence were ignored.
Below is a letter to the relevant BBC team, placing my concerns about the coverage on record:
Letter to BBC News 3 July 2023
The thrust of the BBC reportage was on airing a defunct and empty argument that culture change alone is needed.
Robert Francis commented disingenuously that NHS boards need to “buy into” and “understand” about whistleblowing. He knows full well that many boards understand, but simply choose self interest and suppression. He used to advocate dismissal for abusive NHS CEOs.
Culture change is of course needed but it is not going to happen without enforcement. Road safety laws on safety belts and drink driving are an example of law changing behaviour and culture.
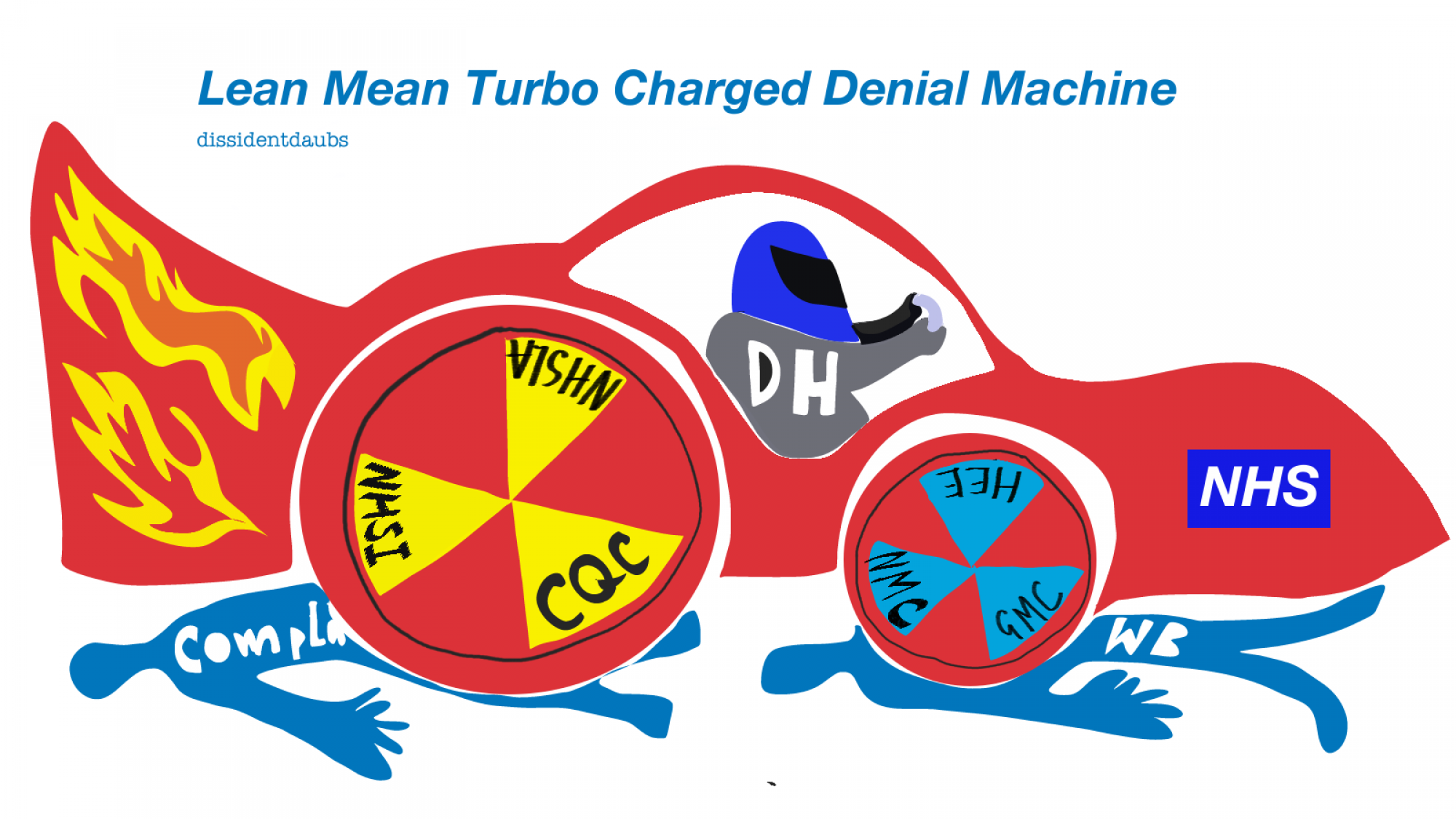
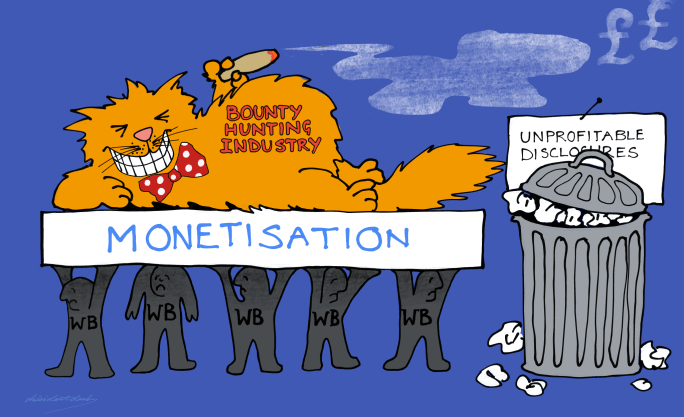
Power, however, naturally fears enforcement of whistleblowers’ rights to protection and action upon their disclosures.
The BBC News coverage appeared the day after The Guardian ran an item featuring the BMA’s call for reform of UK whistleblowing law:
NHS whistleblowers need to be better protected by the law, says BMA
Moreover, BBC News featured the National Guardian’s claims to purportedly support accountability for whistleblower reprisal:
“Dr Chidgey-Clark says the main healthcare regulator – the Care Quality Commission (CQC) – and NHS England itself could do more to protect individual whistleblowers and rein in rogue managers.
“I do call on them to do everything they can within their power to ensure there is accountability and these serious issues are looked into,” she says, “because without that, more high-profile cases will happen and, potentially, more patient harm and worker harm will happen. And in our society, in our healthcare system, we don’t want to see that.”
It is hypocritical of the National Guardian and her Office to call for others to ensure accountability for whistleblower reprisal and detriment, when they have done the opposite.
And why the distasteful focus on “high profile” cases? Every whistleblowing case matters, because every patient matters.
The National Guardian’s Office was primarily set up to provide independent reviews of poorly handled NHS whistleblowing cases, but has conducted a shockingly low number of case reviews since the Office was established in 2016.
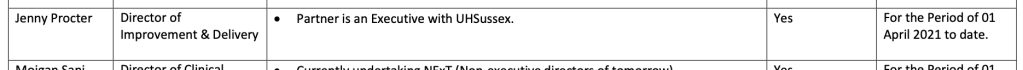
Case reviews by the National Guardian since 2016:
Southport and Ormskirk NHS Trust 2017
Northern Lincolnshire and Goole NHS Foundation Trust 2017
Derbyshire Community Health Services Foundation Trust 2018
Nottinghamshire Healthcare NHS Foundation Trust 2018
Royal Cornwall Hospitals NHS Trust 2018
Brighton and Sussex University Hospitals NHS Trust 2019
Northwest Ambulance Service NHS Trust 2019
Whittington Health NHS Trust 2020
Blackpool Teaching Hospitals NHS Foundation Trust 2021
Thematic review of ambulance trusts 2023
The case reviews turned into toothless systems reviews and are now not even called case reviews anymore. They have been renamed “speak up reviews”, hiding their original purpose.
The NGO’s case reviews have avoided criticising any senior manager for harming whistleblowers.
Occasionally, ineffectual recommendations are made about detriment suffered by whistleblowers, such as the following recommendation at Blackpool Teaching Hospitals in 2021:
“Within three months the trust should:
… 1.12 Communicate that detriment for speaking up will not be tolerated, act to prevent detriment occurring, and put in place procedures that would enable cases of detriment to be looked into effectively when they are reported.”
That is hardly accountability for serious wrongdoing. It glossed over serious harm already done to the trust whistleblowers.
At North Lincolnshire and Goole, where the trust Chair publicly and notoriously attacked a whistleblower, the National Guardian made no reference to this incident in its case review report other than to say that the Chair expressed “regret” and made no recommendation for regulatory action to be taken against the trust Chair.
The NGO case review report for North Lincolnshire and Goole merely stated that a review was carried out because:
“We carried out this review because we had received information that the trust’s support for its workers to speak up did not always meet with good practice.”
Whitewash Central in other words.
In the latest case review by the current National Guardian, which was a thematic review of ambulance trusts, the resultant review report listed grievous examples of detriment (pages 43 and 44).
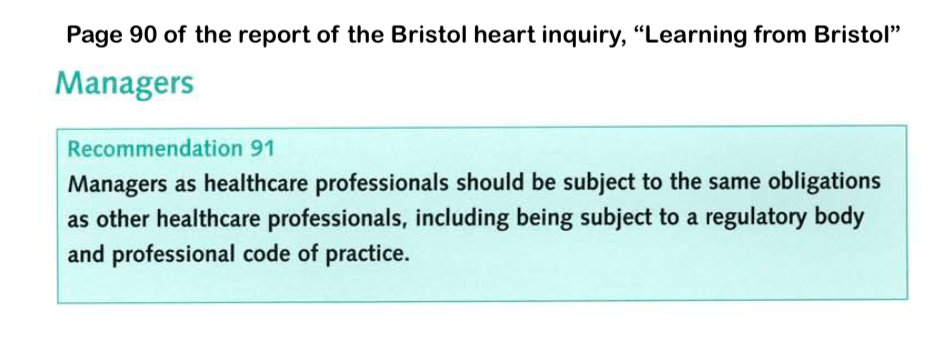
But the National Guardian did not criticise any managers responsible and kicked the can down the road by only suggesting that the Kark review recommendations should be implemented:
“One of the Kark Review recommendations called for processes to ensure greater accountability for leaders, including a focus upon behaviour which suppresses the ability of people to speak up about serious issues in the health service. This recommendation must be implemented as a matter of urgency.”
It was in fact within the National Guardian’s gift, and indeed arguably one of her duties, to request that the CQC review trust directors under Fit and Proper Persons regulation, and that NHS England should take related action. But she did not report that she did so.
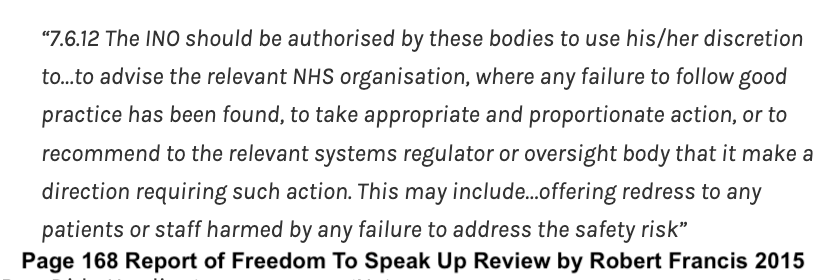
Compounding these failures to hold abusive managers to account and to set the right tone, successive National Guardians have also refused to facilitate access to redress for harmed whistleblowers. This is despite the fact that this was recommended in the 2015 Freedom To Speak Up Review:
The Greasy Freedom To Speak Up Review is Stuck. More Tales of Silence about Silence.
They have repeatedly taken the indefensible line that it is not part of their job.
Unsurprisingly, the National Guardian and her Office are not trusted by the NHS workforce and regularly receive only a tiny number of qualifying disclosures as a Prescribed Person under UK whistleblowing law, from an NHS workforce of 1.4 million.
BBC News reported quite wrongly that the National Guardian’s Office received over 25K contacts last year. This was actually the contacts received by local NHS trust Freedom to Speak Up Guardians and others.
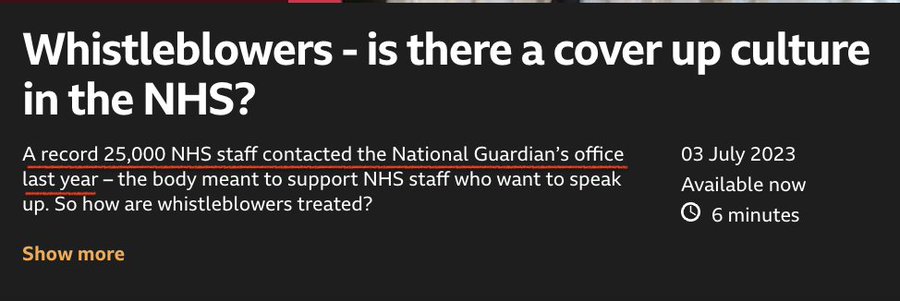
In fact, in 2021/22 the National Guardian’s Office received only 30 qualifying disclosures from 1.4 million NHS staff.
Appallingly, the NGO sent 13 of these 30 staff back to their trusts:
“Signposted a worker to the Freedom to Speak Up Guardian at their organisation, so that the worker could contact them for support to raise matters relating to their disclosure”
When NHS staff contact the NGO (and some of them will be NHS trust Freedom To Speak Up Guardians who have been blocked or victimised for helping whistleblowers), they will have lost confidence in their employers.
It is unsafe and abusive to give such staff the runaround and make them go back to their employers.
Yet the NGO tried this approach in the whistleblowing case of Mr Shyam Kumar surgeon from University Hospitals Morecambe Bay NHS Foundation Trust (UHMBT), despite the fact that this trust was already notorious for several serious whistleblowing failures. This included a trust cover up of breast screening failures.
I am aware of at least seven whistleblowing cases from UHMBT, and yet the NGO has studiously avoided any case review of this organisation.
That must surely be a serious failure in the NGO’s duty of care to trust staff, and another example of the political nature of the NGO in how it sidesteps matters that are inconvenient to power.
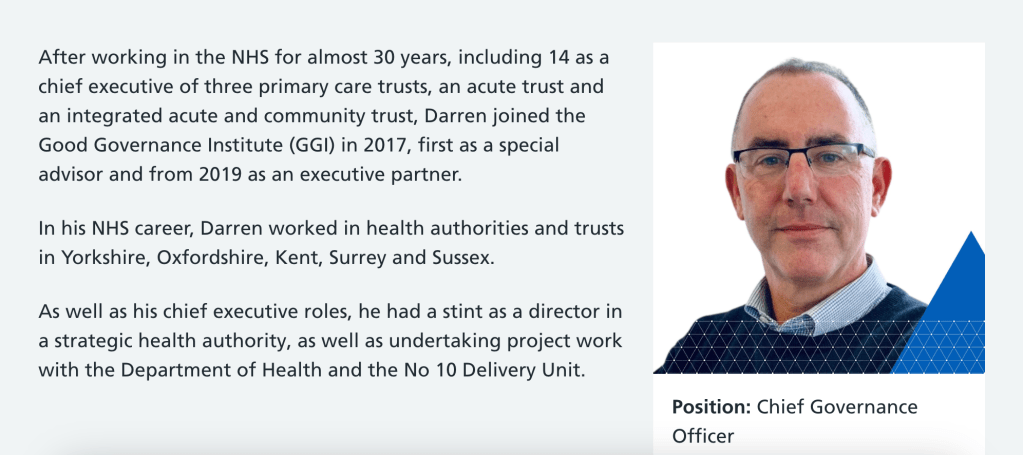
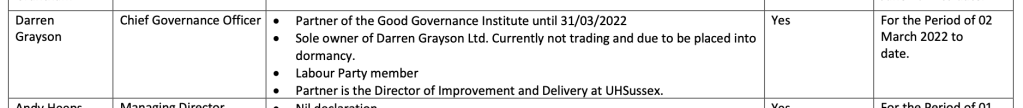
Another well known example is Henrietta Hughes the former National Guardian’s favouritism towards the trust board at Sussex, when she arbitrarily allowed the trust time to “improve” before conducting a review. This had an impact on patient safety and likely helped to delay proper scrutiny of some very serious whistleblower allegations about deaths at the trust. The deaths are now under police investigation.
That is hardly holding erring senior trust managers to account.
I asked Ian Trenholm CQC CEO to investigate the failure of the NGO at Sussex since the police investigation became public knowledge. He passed it to the CQC complaints team, who replied on 5 July 2023:
“After considering your email, we will not be considering this as a corporate complaint, as it goes beyond the time limit of what we would consider under our policy.”
So no accountability.
In the case of whistleblower Dr Jasna Macanovic who asked for help, the National Guardian’s Office told her to come back after her Employment Tribunal had concluded. This meant there would be no help for her or for patients for years. This too has happened to other NHS whistleblowers.
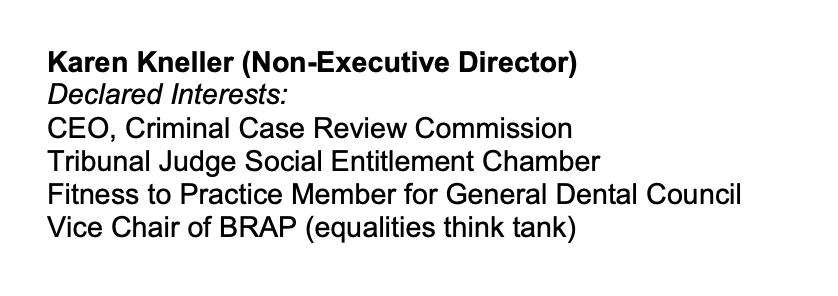
It was left to the whistleblower community to refer Dr Macanovic’s dismissing Medical Director to the CQC (the National Guardian’s employer) under Regulation 5 Fit and Proper Persons, who as usual refused to find any breach of the regulation.
So no accountability.
NGO failure on Jane Chidgey Clark’s watch
And what of similar failings on Jayne Chidgey Clark’s watch, as the third National Guardian?
I have seen correspondence supplied by an NHS whistleblower with a very serious case who was dismissed despite seeking help from their local trust Freedom To Speak Up Guardian.
They contacted the National Guardian’s Office for help. They gave the NGO a detailed account of what had happened to them, including their attempts to seek help through the local trust Guardian.
The National Guardian’s Office, under Jayne Chidgey Clark, wrote back last year suggesting:
“We understand that you were a worker at REDACTED and have attempted to speak up about a number of issues, including those around patient safety. We understand that you do not feel able to speak to the Guardian at the Trust as they are employed by them. However, we would encourage you to contact them if you have not already done so.”
The NGO correspondence continued in this incompetent and insensitive vein, such that the whistleblower questioned whether the NGO had actually read their original request for help.
This is a typical example of how the NGO operates.
The Office resists requests for help, and its first response is to try to send NHS whistleblowers back to the organisations in which they have lost confidence.
Sending victims back to abusers is not a recognised method of safeguarding.
I hope that BBC News will at some point acknowledge that the NGO’s actions smack more of collusion than accountability.
As does the disgracefully low number of case reviews conducted by the NGO.
The National Guardian’s Office simply does not protect whistleblowers.
RELATED ITEMS
The lack of evidence base for the Freedom To Speak Up project
The lack of evidence is examined here:
Strikingly, in the same year that Robert Francis and the government launched the Freedom To Speak Up charade, the “exemplar” trust on which Francis purportedly based the model was criticised by the CQC.
It was reported that the prototype Cultural Ambassador role had disappointed some staff:
“The Staffordshire and Stoke on Trent Partnership NHS Trust created a role of ‘Ambassador for Cultural Change’. This innovative role was designed to allow the staff voice to be heard and concerns from staff to surface in a way that focused on the topic rather than the individual, protecting the identity of any staff member wanting to remain anonymous. This initiative received significant national attention. We saw that not all staff were happy with this role. They were often guarded and concerned they might not have the full protection promised. While some staff engaged with the Ambassador for Cultural Change many felt that the actions from this did not follow on as expected.”
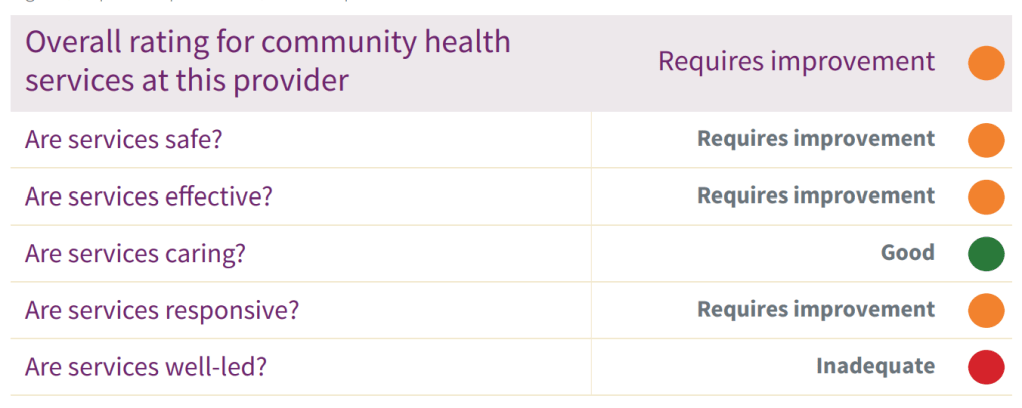
And the trust was rated “Inadequate” on the Well Led domain partly because trust executives had not addressed staff concerns:
Francis et al did not put these salient facts in the glossy Freedom To Speak Up promotional material.
The truth, as ever, struggled to lace its boots whilst its counterpart had already been widely disseminated by government spin doctors.
The Low Fact National Guardian’s Office
The Disinterested National Guardian & Robert Francis’ Unworkable Freedom To Speak Up Project
Sorry is the hardest word: CQC, Paula Vasco-Knight and Regulation 5 Fit and Proper Persons
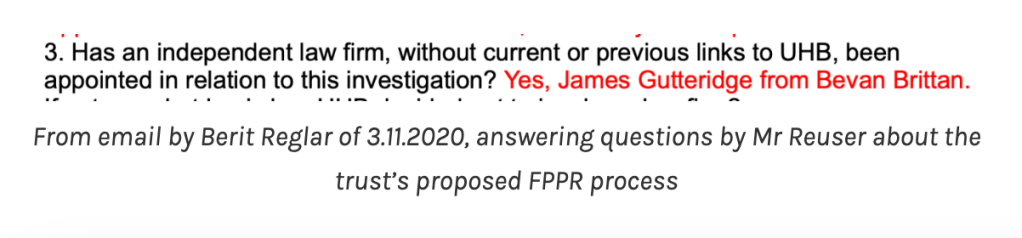
Mr Tristan Reuser’s whistleblowing case: Scandalous employer and regulatory behaviour on FPPR