By Dr Minh Alexander retired Consultant Psychiatrist
25 January 2023
Dear All,
On Monday 23 January I attended a “town hall” style meeting organised by Mike Bewick, the former GP and former NHS deputy Chief Medical Officer of NHS England, who has been appointed by Birmingham and Solihull Integrated Care Board to lead a review into UHB. His appointment followed a series of articles by BBC Newsnight about alleged serious dysfunction at the trust.
Affected individuals attended the meeting, including past and current UHB staff. The meeting was co-chaired by Mike Bewick and Preet Gill the Labour MP for Birmingham Edgbaston.
I attended as someone who has worked with fellow whistleblowers, including UHB staff who do not wish to be identified.
I was horrified by what I witnessed, both in terms of what affected individuals shared and how the meeting was conducted.
Sensitive case details were openly discussed in a very large meeting where many participants did not know each other.
There was a request from Chairs that the meeting contents should be treated confidentially, but there were no means of enforcing this. Once information is shared, it can go anywhere, and often does.
This was an unsafe process with respect to protecting whistleblowers and their confidentiality.
Moreover, Mike Bewick signalled his intention to hold more meetings in group format. He will also hold individual meetings.
Protecting whistleblowers’ identity and the confidentiality of their disclosures is taken very seriously in many jurisdictions because a failure to do so can have devastating longterm effects for the whistleblower and their family.
Under the whistleblowing laws of some countries (Australia, Ireland, some EU countries) it is a criminal offence to breach whistleblower confidentiality, and attempts to unmask a whistleblower’s identity are prohibited.
Whistleblowing can never be guaranteed to be risk free. However, the risk increases with internal procedures where the whistleblower can be identified, potentially allowing reprisal by management.
I consider the ICB’s reviews of UHB to be a de facto internal procedure as they are not sufficiently independent. I anticipate that information will be shared amongst the NHS bodies, one way or another.
I am aware of several occasions when the CQC has broken whistleblower confidentiality and one occasion when the CQC (unsuccessfully) solicited information for the purpose of discrediting a whistleblower during legal proceedings. I am also aware that NHSE has let down whistleblowers, both its own and those in provider organisations.
The way the meeting on 23 January was conducted confirmed my concerns that confidentiality will not be adequately protected.
From my overview of NHS whistleblowing cases across a range of organisations, both providers and oversight bodies, and the sometimes negligent, complicit or even abusive behaviour of regulators, I do not believe that any NHS controlled review of UHB can be truly independent or rigorous.
I also believe that contributing directly to such a review will place UHB staff at greater risk of reprisal.
Instead, I would advise making your disclosures to the media on an anonymous basis or with agreement that your confidentiality is protected. Alternatively, make a similar disclosure to a trusted local union branch with a track record of raising concerns. Not all local unions branches necessarily help whistleblowers, so research in advance. The advantage of raising concerns through a union is that individuals are less likely to be targeted. Collectively raised concerns which demonstrate patterns are especially powerful. The UNISON UHB dossier that was sent to CQC, which strongly corroborated existing concerns that UHB was intimidating doctors who raised concerns, is an excellent example.
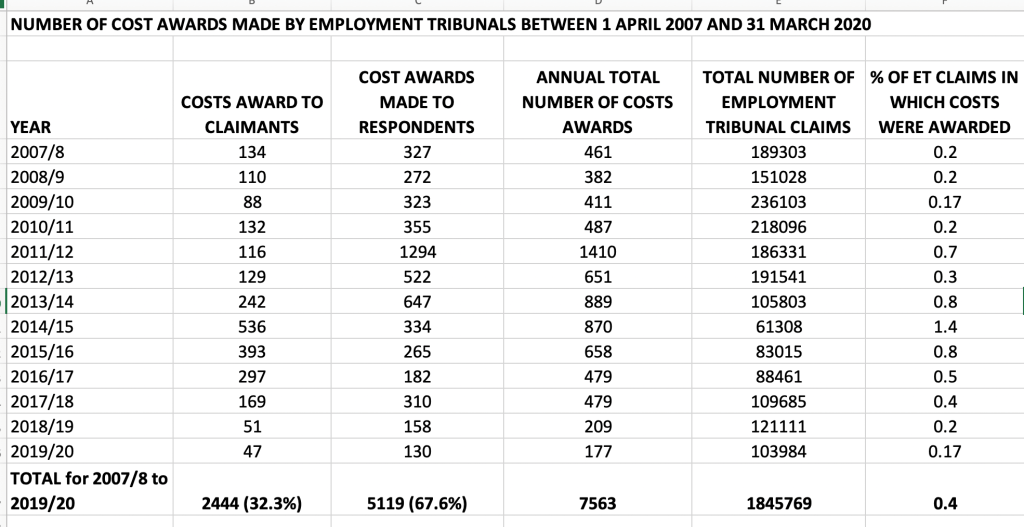
Not going through an internal route of whistleblowing has potential legal implications if you wish to make a claim to the Employment Tribunal in future, so take advice. However, anonymous or otherwise untraceable whistleblowing means that you are unlikely to suffer victimisation, and you will not need to make a claim at all to the Employment Tribunal, saving you and your loved ones years of pain. Lives can be ruined by a bad whistleblowing experience.
Unless you can afford to be identified – perhaps if you are near retirement etc…I would not risk reprisals.
If you have already spoken up on an identifiable basis, you can make yourself less of a target if you wish, by not pressing your concerns further with UHB and the regulators. If your concerns have not been addressed, you can keep the media informed of this, with agreement that you will not be identified, including indirectly through any potential details reported.
Some may ask: “What can the media do?”
Whistleblowing to the media is not an end to itself, but it can be a way for UHB staff to communicate with power without exposing themselves to reprisal.
It can also be a means of negotiating for a better, properly constituted inquiry into what has gone wrong at UHB.
The Mid Staffs disaster was initially investigated with a non-statutory inquiry. Sustained campaigning led to a statutory public inquiry.
Similarly, hundreds of deaths at Essex Partnership mental health trust recently led only to a non-statutory inquiry. After a boycott by bereaved families and staff, the government is now being asked to rethink this.
Importantly, a statutory inquiry will be more likely to deliver accountability for the issues at UHB. NHS regulators have a notorious history of protecting and recycling failing NHS managers. At present NHS England (which has oversight of the ICB’s reviews of UHB) and the Secretary of State are in the process of watering down the Kark Review recommendations on protecting NHS staff and patients from poor managers. Any review of UHB controlled by NHS England will not deliver true accountability for the failures.
Also, be aware that UHB is especially sensitive as it represents a failure to learn from Mid Staffs. There has already been one re-run of Mid Staffs at Liverpool Community Health NHS Trust, where a rush to Foundation status under Jeremy Hunt’s watch led to a disaster. This resulted in an investigation report by Bill Kirkup, which in turn led to the the Kark recommendations for tighter scrutiny of NHS managers. And yet we now have a further serious failure of management culture, at UHB, after NHS England and the government failed to learn and act.
There is every reason for the establishment to minimise what has happened at UHB.
If you want a better, more powerful inquiry which will handle evidence much more safely and formally, and which can protect vital witnesses including gagged former UHB staff, compel disclosure from senior witnesses, and has a greater chance of delivering accountability, ask for this through the media and the unions.
You are not obliged to cooperate with or to accept the ICB’s proposed reviews.
I attach below a letter from three senior medics and ex UHB employees:
Manos Nikolousis, Chairman Medical School EUC, Associate Professor Haematology
Professor John Watkinson, Consultant ENT Surgeon
Tristan Reuser, Consultant Opthalmic Surgeon
who have written to local MP Preet Gill and Healthwatch Chair Richard Burden, to set out their concerns about the independence of the reviews commissioned by the ICB.
Please do protect yourselves and your families in these difficult times.
Experienced whistleblowers watch the unfolding events at UHB and send all our good wishes, and also our hopes that you can avoid the pitfalls.
All my very best.
Minh
Dr Minh Alexander
NHS whistleblower and retired consultant psychiatrist
Cc
BBC Newsnight
Unite the union
UNISON
HCSA
RCN national and local offices
Royal College of Midwives
BMA
GMB
Chartered Society of Physiotherapy
Federation of Clinical Scientists
British Association of Occupational Therapists
Society of Radiographers
Yve Buckland Interim Chair UHB
Patrick Vernon Interim Chair Birmingham and Solihull ICB
Mike Bewick
Preet Gill MP Birmingham Edgbaston
Richard Burden Chair Healthwatch
Steve Barclay Secretary of State
Parliamentary Health and Social Care Committee
Tahir Ali MP Birmingham Hall Green
Liam Byrne MP Birmingham Hodge Hill
Khalid Mahmood MP Birmingham Perry Barr
Steve McCabe MP Birmingham Selly Oak
Jess Phillips MP Birmingham Yardley
Gary Sambrook MP Birmingham Northfield
Shabana Mahmood MP Birmingham Ladywood
LETTER BY MANOS NIKOLOUSIS, JOHN WATKINSON AND TRISTAN REUSER ABOUT THE BEWICK REVIEW
16-1-2023
To
The Rt Hon Preet Kaur Gill MP
Mr R Burden, Chair , Healthwatch Birmingham
Thank you both for your continued involvement in this matter. We are contacting you again following our discussions with you last week as well as fresh revelations by the BBC on Friday 13th January about the management and culture at UHB, damaging patient safety and staff morale. These revelations were of such a serious nature that soon demands were made for an independent inquiry, which only grew stronger once the scale of the problems became clear and more facts surfaced such as a Unison report about UHB, which made a comparison with the Mid Staffs scandal.
The ICB reacted to the initial allegations by immediately commissioning three reviews, which In our view are not fit for purpose. In this letter we will focus particularly on the first review, led by Mike Bewick.
Summary:
–We have grave concerns about the ICB’s reviews into UHB, which were extraordinarily commissioned in haste without involving those most seriously harmed by toxic trust management actions.
-We are concerned that a review by an NHS insider, overseen by NHS bodies with conflicts of interest, is woefully inadequate for the task and will seriously fail patients and staff.
-We believe that the haste and direction of the ICB’s reviews are aimed at controlling the narrative, and not a genuine resolution. The current Terms of Reference are unacceptable to us.
-The Secretary of State is reported to be reassured that NHS England is in overall control, but NHS England’s West Midlands region has a history of serious failures, including Mid Staffs, maternity failings at Shrewsbury and Telford, unsafe care at Worcestershire Acute and the Ian Paterson breast surgery scandal at Heartlands.
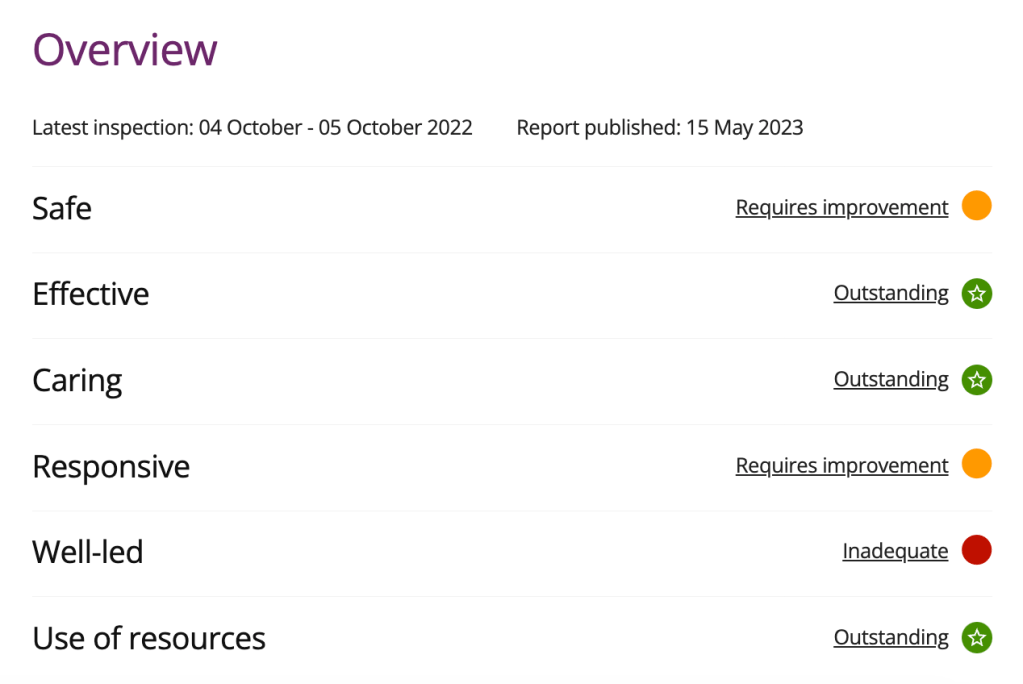
-UHB is a story of closed cultures and systemic failures, including by the regulators. The CQC in particular had a chance to stop the toxicity years ago and failed to disclose important data, such as a damning dossier sent to it by UNISON.
-The detail of the BSol ICB’s arrangements for a review betray a fundamental lack of understanding of the problem. Moreover, UHB’s public response to the scandal reveals an organisation still in denial. The current plans will not surmount these difficulties: only a forensic, external and independent investigation will enjoy the confidence of UHB’s victims and the public at large.
Our objections against the Bewick review include:
1. The involvement of Birmingham and Solihull Integrated Care Board (ICB)
1.1 The reviews are commissioned by the ICB board, which has strong links with UHB. There is a clear conflict of interest here:
-As commissioner of healthcare for the local population, BSol CCG, the recent forerunner of the inchoate BSol ICB, neglected to treat the performance failings of its biggest acute provider (UHB) with anything like the attention they required.
-The former CEO of BSol CCG, Paul Jennings, is now a non-executive director at UHB.
-Two BSol ICB Board members are former senior employees of UHB.
1.2 David Rosser, the previous CEO of UHB, was offered a new position as regional strategic director for Digital Health and Care at a time that UHB ranked 119 out of 120 in the table of English hospital trusts, its cancer waiting times were among the worst in the country, and UHB had the country’s longest waits for cardiac surgery, resulting in devastating impact on patient care. Additionally, while David Rosser was at the helm, the trust’s own Freedom To Speak Up Guardian referred to a climate of fear and bullying in his report. As you rightly stated: “There has been a clear failure of leadership, a failure of governance and a failure of regulation.” The ICB declared in its notes of its latest board meeting dated 9 January 2023 that the ‘contribution David made….leading the system through an unprecedented period was enormous’.
1.3 David Rosser’s new role within the region will mandate a continued close working relationship with BSol ICB and he remains in a position to influence the review. We understand that the ICB was involved in his recent appointment and that after starting his new role, David Rosser was still invited to attend the above meeting of the ICB. The lack of transparency and detail about David Rosser’s new role, his appointment, the funding of his post and links to the ICB undermines accountability and public confidence in this review.
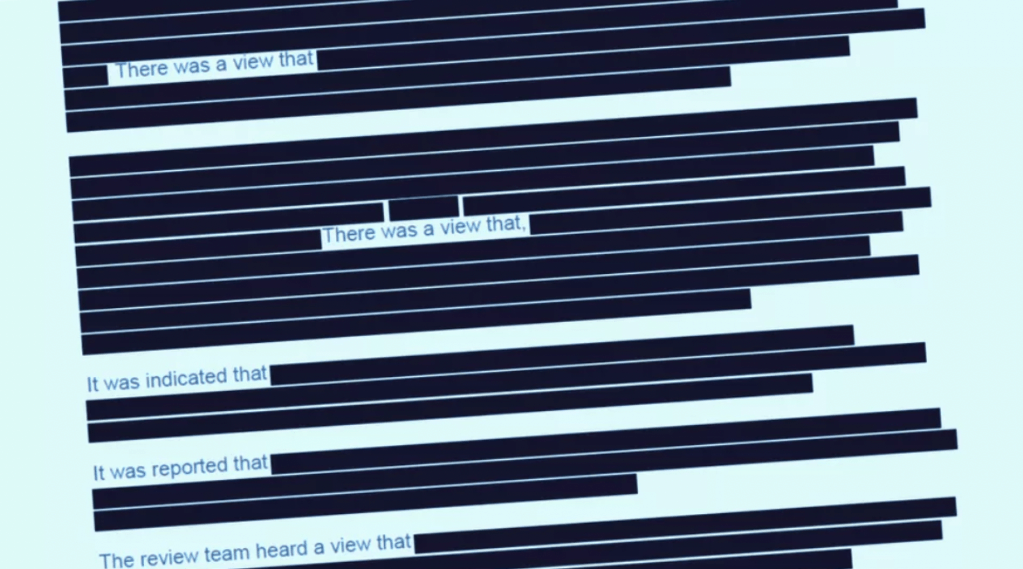
1.4 As the ICB review is not a public inquiry with statutory powers, its chair does not have the power to ungag (ex) employees who have signed non-disclosure agreements. As it is known that UHB has used these clauses to silence (ex) staff, their voices won’t be heard in this review.
1.5 Preet Gill’s letter to Steve Barclay MP also argues convincingly why an independent inquiry is needed instead of an ICB led review.
2. The appointment of Mike Bewick
2.1 Mike Bewick, who used to work for NHSE as Deputy Medical Director, is very much part of the medical and NHS senior establishment. Despite the fact that various regulators and medical institutions, such as the CQC and NHSE, were or should have been aware of the problems at UHB, they took no or insufficient action. The fact that the CQC did not disclose a UNISON report which corroborated our concerns only highlights the possible complicity of the regulators, a recurring theme in other NHS scandals. For these reasons, Mike Bewick is unsuitable to lead any review of UHB.
2.2 Even if Mike Bewick does not have direct links with UHB/ Dr Rosser, his indirect connections are reason for concern in our view :
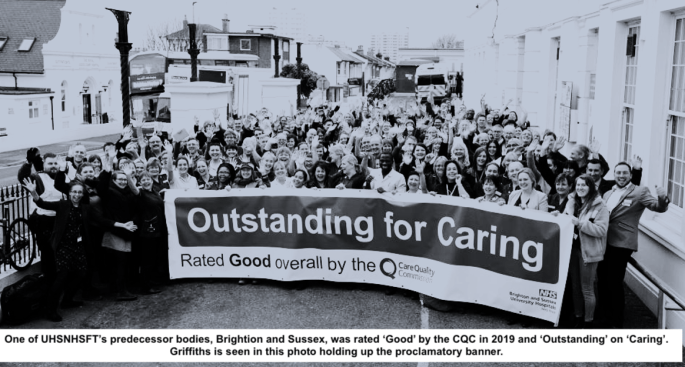
-Mike Bewick was Bruce Keogh’s deputy at NHS England. Bruce Keogh used to work at UHB (1996-2004).
-Bruce Keogh and David Rosser were colleagues at UHB and they co-authored an article together on Weekend Mortality.
-Mike Bewick and Dame Julie Moore, previous CEO of UHB, are current members of the Centre for Progressive Policy Advisory group.
2.3 As a former Deputy NHS MD (to Professor Sir Bruce Keogh), Mike Bewick is poorly placed to undertake an unprejudiced review: there is a risk of bias, if only unconscious, resulting from not only his duties as an NHSE employee but his discussions with Bruce Keogh as an ex-UHB employee.
2.4 Moreover, we understand that Mike Bewick has reportedly made comments which suggest he had pre-judged the outcome of the reviews already, and seems to be thinking about splitting UHB up. This would be a deflective manoeuvre. It is the toxicity of the management culture that is the issue, not the size of the trust. Other trusts of a similar size have not had the same problems. If it is true that there are signs of a pre-determined outcome, this again suggests that Mike Bewick is not suitable to lead this review.
2.5 Had we been consulted, we would have made clear that the appointment of a senior NHS insider was completely unacceptable because of inherent conflicts of interest. An independent inquiry, led by a truly impartial outsider such as a judge, would be far more suitable to deal with the scope and nature of the concerns about UHB.
3. The current Terms of Reference are unacceptable to us
3.1 To the best of our knowledge none of the victims of UHB’s behaviour have been invited to participate in the drawing up of the ToR. This is not only disrespectful but also a missed opportunity to ensure effective ToR through discussions with those who have first hand experience of the culture at UHB and the impact on staff.
3.2 According to the first term of reference the findings of the report drafted by Mr Nikolousis into concerns over the care of patients with haematological conditions will be reviewed with UHB haematologists to determine whether further expert review should be recommended. BSol ICB demonstrates no understanding of the problem of a dysfunctional department. We understand that the report should be shared with the members of the department but they should not be granted the power to veto the commissioning of any further external investigation.
3.3 Additionally the second term of reference refers to ‘the appropriateness of the governance processes which apply when determining whether or not to make a referral to a professional regulator such as the GMC, including an overview of the TR case’. Again, BSol ICB demonstrates little understanding of the issues, of which the decision to refer to a professional regulator is just one small strand. This is too loosely written and we believe this is a consequence of a lack of ICB consultation with those of us who were subject to referrals.
3.4 Emphasis must be placed on a detailed examination of each element of such cases including, inter alia, the timing of the referral; the accuracy of the content of both the referral and subsequent communications. The ICB terms of reference are too weak and non-specific to explore biased and or malicious management behaviour.
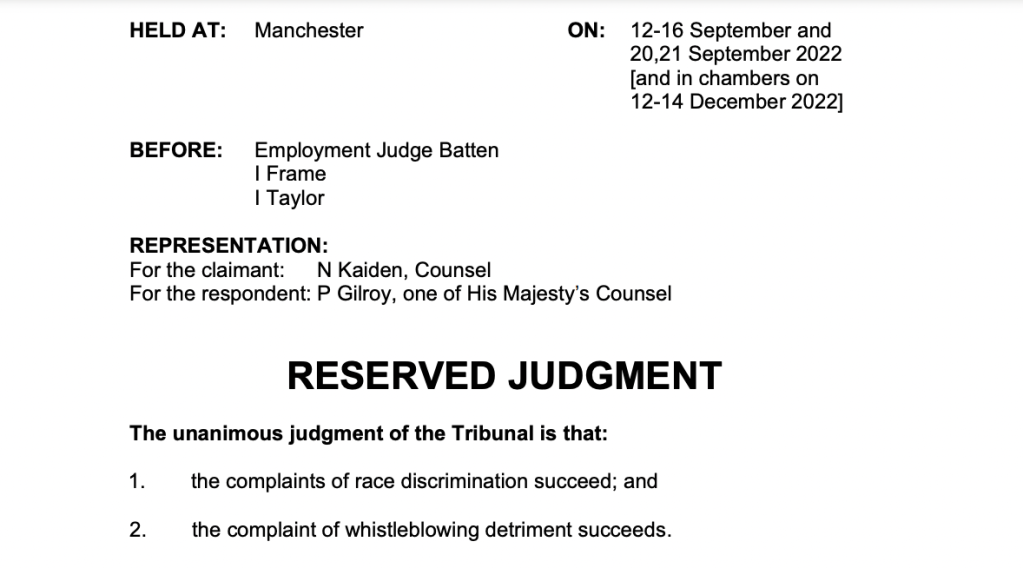
3.5 The ToR also miss out a critical issue: a flawed Fit and Proper Person process by the trust on David Rosser. The trust has admitted to at least one FPPR review in response to multiple referrals to the CQC under Regulation 5. The trust appointed a subordinate to investigate David Rosser, someone who was not even a board member, and she was assisted by a lawyer from Bevan Brittan, a firm retained by the trust. Additionally, the MHPS designated board member in the Tristan Reuser case, was also involved in the FPPR investigation. This was therefore the opposite of an independent exercise. David Rosser was deemed to be a Fit and Proper Person despite his behaviour relating to Tristan Reuser’s MHPS investigation, dismissal and employment case, including misleading the regulator for which Dr Rosser received a GMC warning. Had the ICB consulted with us, we would flagged the FPPR matter as another area for investigation.
3.6 The CQC had a chance to stop the bullying and toxicity at UHB years ago, when the FPPR referrals were first made about UHB but failed to do so. It follows that a localised review of UHB which does not even look at FPPR issues, let alone at any regulatory actions, will hardly scratch the surface of the truth.
3.7 As flagged at the meeting with Richard on 13 January, there are concerns about financial transparency at UHB, which stopped producing routine financial transparency data after 2017. The trust persisted with this despite run ins with the ICO after complaints by the public who filed FOI requests and questions have to be asked about this financial secrecy. We would have raised this with the ICB had they troubled themselves to consult us.
3.8 The ICB of course is conflicted in this matter and in general, as it too had a responsibility in its predecessor form for oversight of UHB’s performance.
3.9 Finally, the Terms of Reference extend well beyond the core issues to embrace other matters that are already well documented. This represents a wasteful distraction from the allegations that the review should focus on, if not wilful obfuscation.
4. Methodology
4.1 There is no reassurance that all victims will be offered a confidential interview.
5. Conclusion
5.1 In our view, Birmingham and Solihull Integrated Care Board took precipitate action without involvement of all stakeholders in order to fully control the process and therefore the outcome. This is unacceptable.
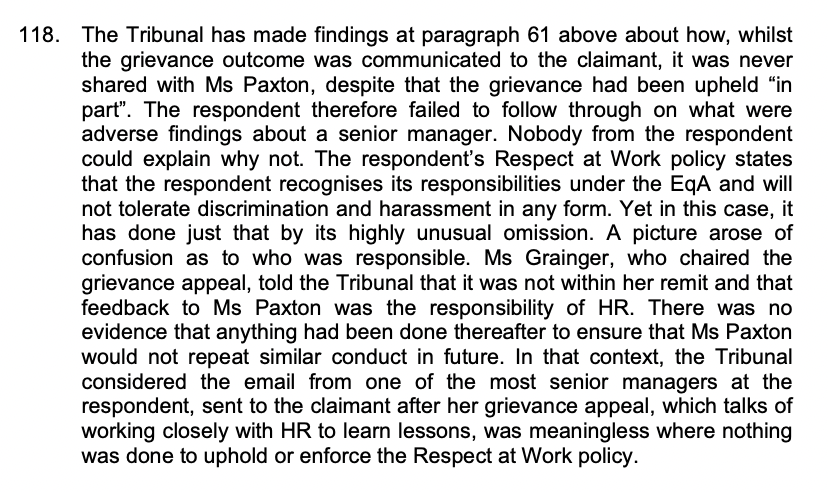
5.2 The impact of UHB’s actions on victims’ lives and the effect on patient safety cannot be underestimated. Careers have been destroyed and families damaged by the emotional, health and financial and health problems that ensued. We have fought for many years to uncover and then expose the truth. Having been largely ignored by the NHS and its regulators we have finally achieved this only with the help of the media. Now that our concerns have been recognised, it is incumbent upon us to ensure that they are appropriately investigated: independently, and without fear or favour. We owe this to ourselves, our families and UHB’s staff. Most of all we owe it to the patients at UHB whose safety has already been compromised and those at future risk.
5.3 It is surely clear to everyone, including BSol ICB, that the very nature of a central allegation, that there exists at UHB a “mafia-like culture”, demands a truly independent investigation. You have, quite rightly, called for this yourself. The current position is thus unacceptable to us. We would urge you both to use your influence in order to generate an investigation that will enjoy the confidence of all.
We ask you politely to forward our letter to all those who have approached you, so they are able take note of our concerns.
Yours sincerely,
Manos Nikolousis, Chairman Medical School EUC, Associate professor of hematology
Prof John Watkinson, consultant ENT surgeon
Tristan Reuser , consultant ophthalmic surgeon
CC
Parliamentary Health select committee:
Steve Brine MP
Paul Blomfeld MP
Martyn Day MP
Mrs Paulette Hamilton MP
Rachael Maskell MP
Taiwo Owatemi MP
Lucy Allan MP
Paul Bristow MP
Chris Green MP
Dr Caroline Johnson James Morris MP
Steve Barclay, Secretary of State for Health and Social Care, MP
RELATED ITEMS
Sorry is the hardest word: CQC, Paula Vasco-Knight and Regulation 5 Fit and Proper Persons
HSIB whistleblowers and the Secret King’s Fund Fact Lite report
Mr Tristan Reuser’s whistleblowing case: Scandalous employer and regulatory behaviour on FPPR
Fundamental failure of the NHS Freedom To Speak Up Project: Dr Rajai Al-Jehani unfairly sacked by Royal Free NHS Foundation Trust for whistleblowing on breaches of Human Tissue law, with suppression of linked investigations by University College London
The National Guardian’s Office finally apologises for a breach of whistleblower confidentiality but fails to demonstrate sufficient learning