Last month there was a highly significant press report on the fact that UHMBT has allegedly failed to refer serious maternity cases to the coroner.
Disgracefully a bereaved couple, Sarah Robinson and Ryan Lock, were forced to refer the death of their baby Ida at UHMBT to the coroner, because the trust had failed to do so.
This was despite the fact that expert reports had identified “a catalogue of concerns” in Ida’s care.
The couple reportedly endured a “four year fight”:
The Senior Coroner for the area James Adeley expressed concern that Ida’s parents were forced to report matters to the coroner because the trust had failed to do so:
“Coroner Dr James Adeley told a pre-inquest hearing in Preston this week he was concerned it had been left to Ida’s parents to report her death to his office after hospital managers failed to do so.”
Importantly Dr Adeley observed that, to his recollection, UHMBT had failed to refer any baby deaths since the Kirkup report on maternity failures was published in March 2015.
“He said he was worried ‘systemic’ problems in maternity care identified by Dr Bill Kirkup in March 2015 had not been addressed. He said he could ‘not recall’ a single baby death being reported to him since.
Dr Adeley said. ‘There’s no indication that matters identified in the Kirkup Report have been addressed before this case. That suggests a lack of learning from the report continues to exist, and continues to place lives at risk.’
UHMBT was previously criticised for collusive staff responses to coroners’ inquests, as noted in Kirkup’s report:
“1.93 The coroner made strong criticisms of both the clinical practice and conduct of Trust staff, including collusion in preparation for the inquest and possible destruction of evidence already discussed. Following a Rule 43 letter from the coroner expressing these concerns…”
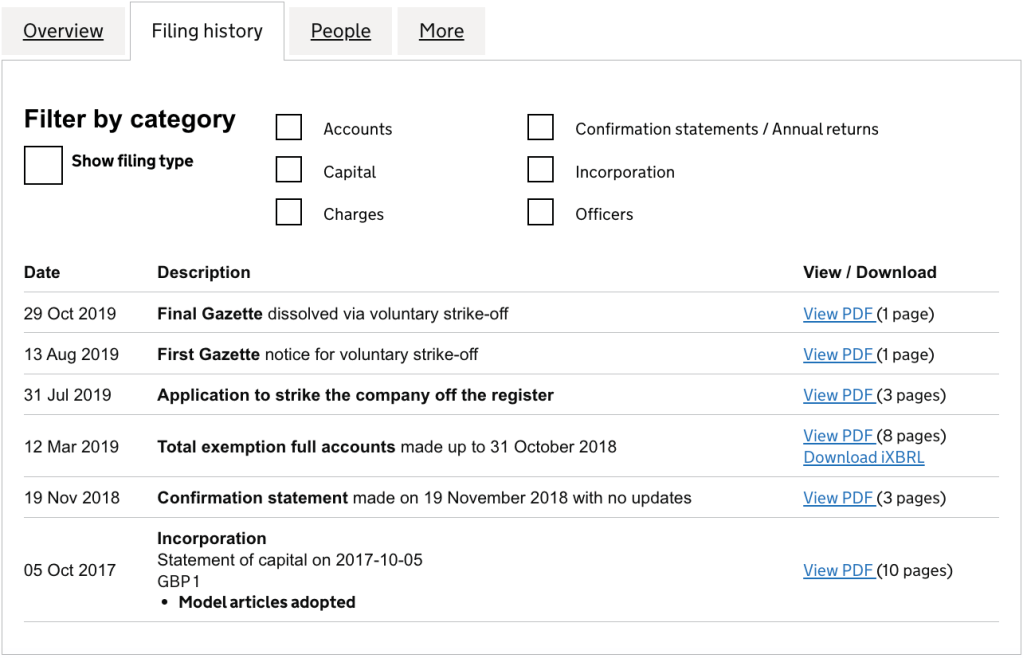
I therefore asked the trust via FOI for information on serious maternity incidents, related referrals to the coroner and the HSIB maternity investigation programme and the trust’s documented claims about the safety and governance of its maternity services, as submitted to the NHS Resolution Maternity Incentive Scheme.
I asked for data from 2015 onwards, following the publication of Bill Kirkup’s report of the inquiry into maternity deaths at UHMBT.
The trust delayed the FOI process by twice asking about definitions of the serious incidents, when these definitions are standard and the basis of routine data submissions to the centre.
The trust has now responded with an obfuscatory reply.
This is the trust’s FOI response of 26 October 2023:
In brief, instead of giving total numbers of serious maternity incidents and total numbers of referrals to HSIB, the trust has avoided this by giving yearly totals and claiming that numbers in some years were too small to reveal.
Crucially, the trust has refused to disclose at all:
- How many investigations of baby deaths have been shared with bereaved families
- How many baby deaths have been referred to the coroner
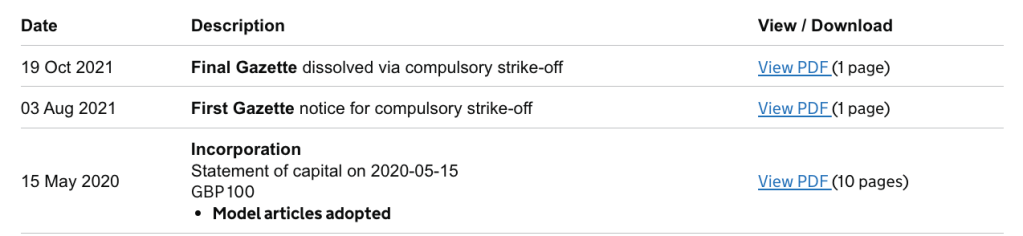
The trust’s data indicates there have been at least 23 baby deaths at UHMBT since 2015, although the precise figure is not yet disclosed.
There seem to have been more baby deaths since 2018:
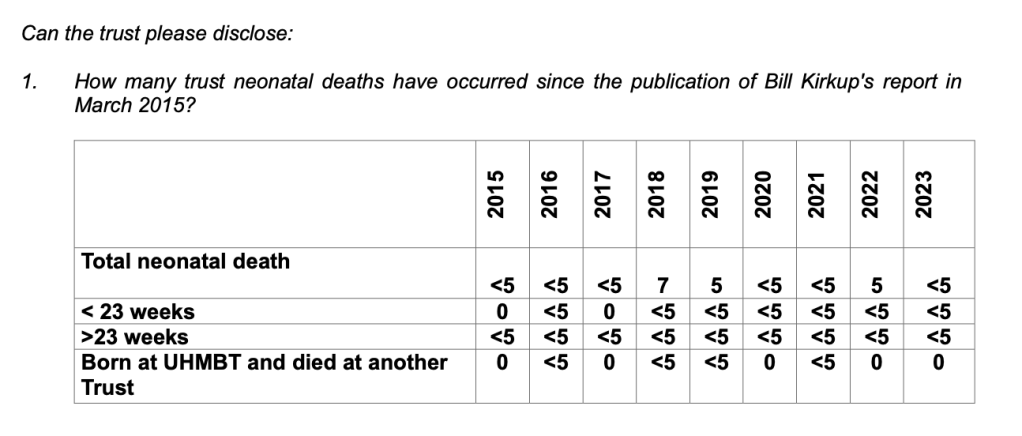
UHMBT claims that it would take too much time to retrieve the data on the number of baby deaths referred to the coroner and doing so would breach FOI limits:
“5. How many of these neonatal deaths have the trust referred to the coroner?
Due to the amount of time to answer Question 3 would be >10hours. To answer Question 5 would be an additional >10 hours. Therefore we estimate in excess of 20 hours to answer these two questions. This does not include the time it has taken to respond to the questions we have provided the information for. The Trust has used multiple systems since 2015 and a review of each care record would need to take place. This information is not held centrally and would require a review of every healthcare record.”
So extraordinarily, the trust asks us to believe that it does not track and cannot tell how many baby death it has referred to the coroner. This could imply appalling governance and failure to learn after an inquiry which slammed its maternity practices, including honesty in interactions with the coroner.
The alternative conclusion being that the trust is not being truthful in claiming that Section 12 FOIA cost exemption applies.
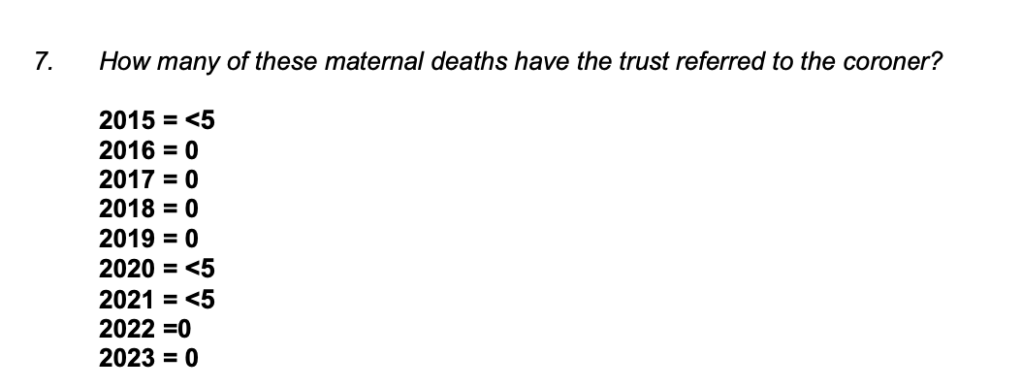
Although the trust claims it is unable to say how many baby deaths were referred to the coroner, it can say that maternal deaths were referred to the coroner in 2015, 2020 and 2021 (albeit without disclosing the actual numbers).
Because of UHMBT’s incomplete disclosure, it is also not clear how many of the trust’s baby deaths were referred to HSIB. At the very least, four referrals were made out of at least twenty baby deaths from 2018 onwards (when the HSIB maternity investigation programme was launched).
Also, the trust failed to disclose requested copies of its submissions to NHS Resolution’s Maternity Incentive Scheme, and instead gave very crude summary data that appears to be raw scores of compliance. Thus, it avoided revealing meaningful detail.
I have written to Aaron Cummins UHMBT CEO, 2012 to present, to ask for a valid response to my FOI request. I copied this to the Senior Coroner.
I received a response from Cummins nine minutes after sending my letter, advising me that a response would be provided “as soon as possible”.
Any further data received from UHMBT will be posted here.
In the meantime, this is a disclosed copy of the UHMBT policy governing the trust’s interactions with the coroner’s office:
UHMBT FOI disclosure: Medical Examiner’s Office Process
These are the salient passages:
- Section B Coronial Cases
4.1.3.39 Ministry of Justice Guidance
Guidance for registered medical practitioners on the Notification of Deaths Regulations (publishing.service.gov.uk)
For registered medical practitioners on the Notification of Deaths Regulations March 2022 sets out the circumstances in which a death should be notified to the Coroner. In addition, the Lancashire Senior Coroner and Regional Medical Examiner has issued a Standard Operating Procedure for referrals to Coroner (see section 5 form 4)
4.1.3.40 Cases identified as potentially Coronial by MEO/QAP/ME should be jointly discussed. Taking into account local guidelines (see section 5 form 4) and Ministry of Justice Guidance
4.1.3.41 If there is agreement that it should be referred to Coroner then case should be discussed with Coroner’s Officer highlighting reason for referral and whether a cause of death can be offered in Ulysees B6
4.1.3.42 Where there is still uncertainty whether Coroner referral is appropriate the ME can contact the coroner to discuss case.
4.1.3.43 It is anticipated that usually in practice, it will be the practitioner who is qualified (QAP) to complete the medical certificate cause of death (MCCD) who will be making the notification to the senior coroner.
4.1.3.44 To facilitate referral the ME Service will where necessary complete Deceased Details (icasework.com) and include ME scrutiny and QAP Death Summary
4.1.3.45 Where the death is clearly unnatural it may be more appropriate for a notification to be made to the senior coroner straight away by the Consultant responsible for the patients care.eg where the Police are involved
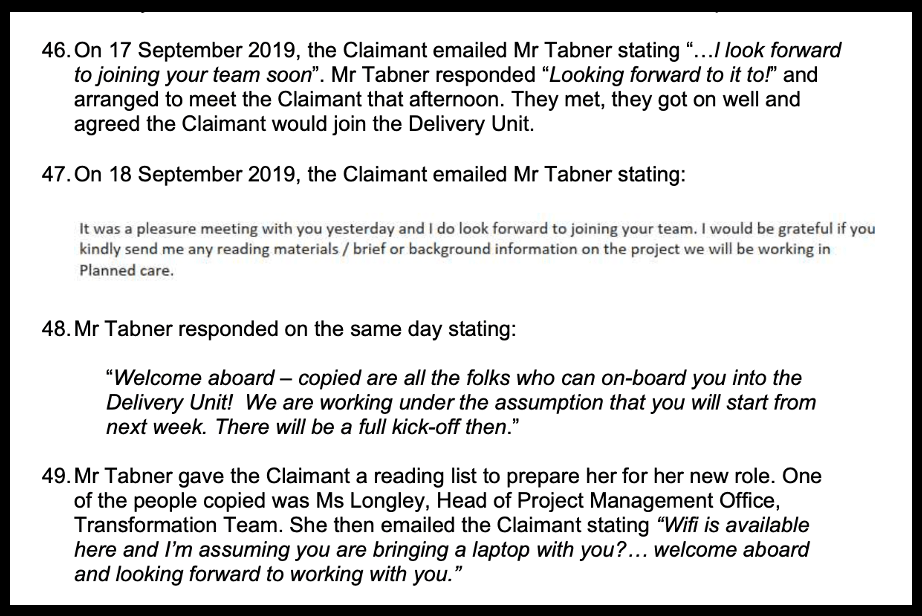
4.1.3.46. Regulation 4(1) requires the notification to the senior coroner to be made as soon as is reasonably practicable after the medical practitioner has determined that the death should be notified.
4.1.3.47 While the regulations do not prescribe a specific time limit for notifications this notification should be prioritised. If the death arises from an event or occurrence that may be suspicious then the police should be informed immediately.
4.1.3.48 A death may have already been reported to the coroner by a person other than a medical practitioner, such as a friend or family member of the deceased, or the police. Such reports will not usually include the information required at regulation 4(3) and (4), and may not provide the coroner with the full medical picture.
4.1.3.49 Therefore, even if a medical practitioner is aware that someone other than a medical practitioner has reported a death to the coroner, the registered medical practitioner should still make a notification under the Regulations
4.1.3.50 The medical practitioner should usually take reasonable steps to establish the cause of death before notifying the coroner. This may include seeking advice from another medical practitioner, such as a medical examiner or any other responsible consultant.
4.1.3.51 If in opinion of ME case should be referred to Coroner and QAP wants to issue MCCD and does not want to refer to Coroner the QAP should be advised to discuss case with their senior Colleague.
4.1.3.52 If the ME and Consultant responsible for patient care cannot reach agreement and the ME still thinks it is appropriate to refer the case to the Coroner then the ME should discuss the case with another ME or Lead ME, or if necessary, in their absence Regional ME.to agree next steps.
4.1.3.53 A coroner’s investigation may not be necessary in all notifiable cases.
RELATED ITEMS
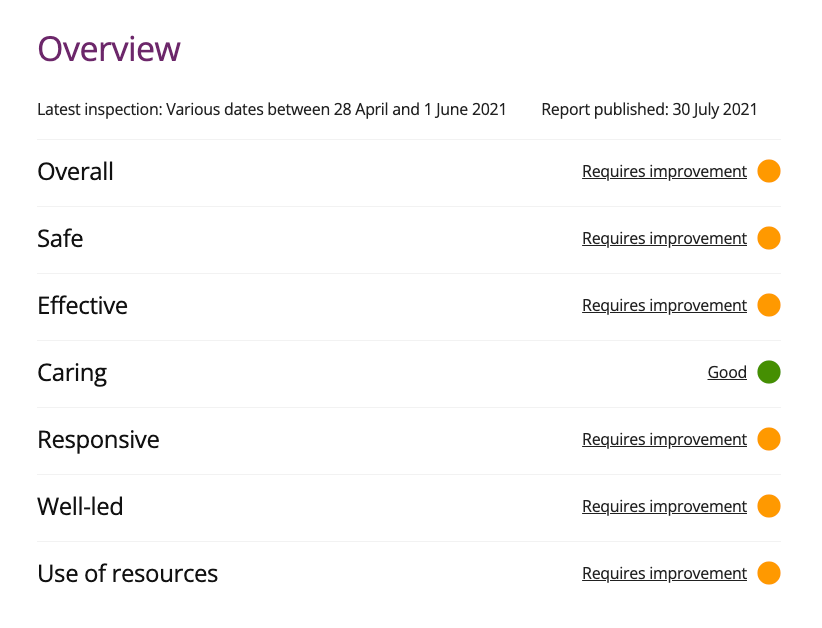
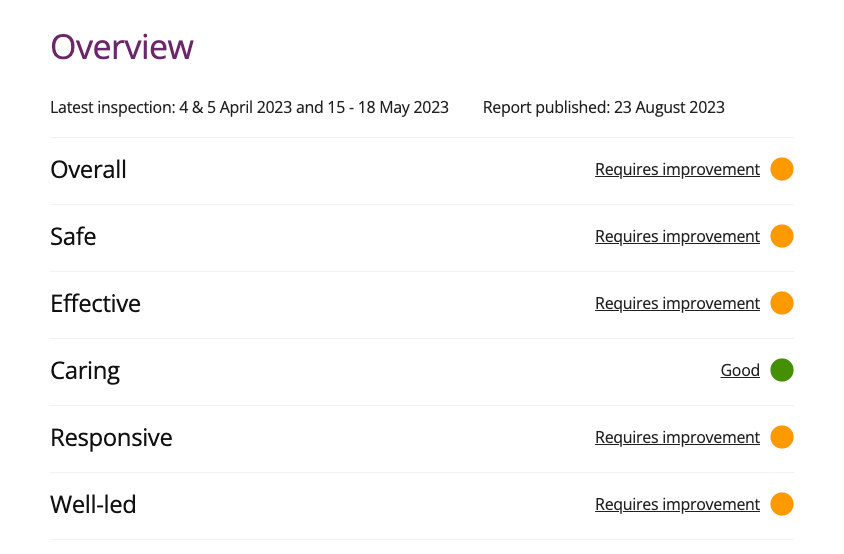
UHMBT is currently rated “Requires Improvement” by the Care Quality Commission, including on the Well Led domain.
UHMBT has been the scene of repeated whistleblower reprisals and gaggings, going back many years. I cite a few of the cases.
Breast screening whistleblowers were harmed and gagged by UHMBT.
Public Health England confirmed in 2015 that their concerns were valid:
External review into North Lancashire and South Cumbria Breast Screening Programme
Litigation continued about the gagging.
A recent case is that of Mr Shyam Kumar, who was doubly harmed both as a trust and a Care Quality Commission employee, after he whistleblew about the unsafe surgical practice of another trust surgeon and other matters.
Tulloch report 2020 on orthopaedic safety at UHMBT (page 60 onwards)
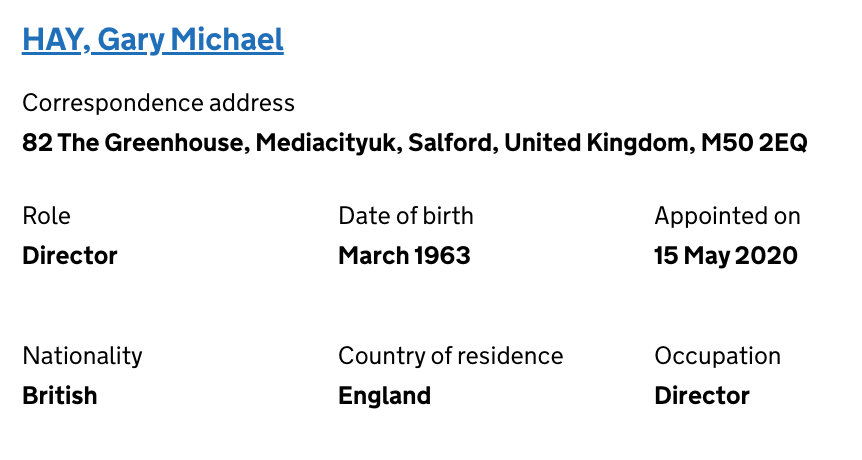
But despite the trust’s questionable governance, it loomed large as a key tool in Jeremy Hunt’s campaign to present himself as a patient safety champion.
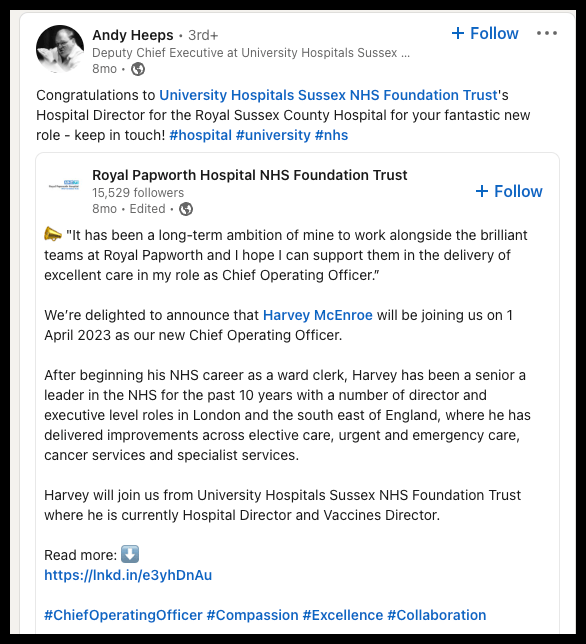
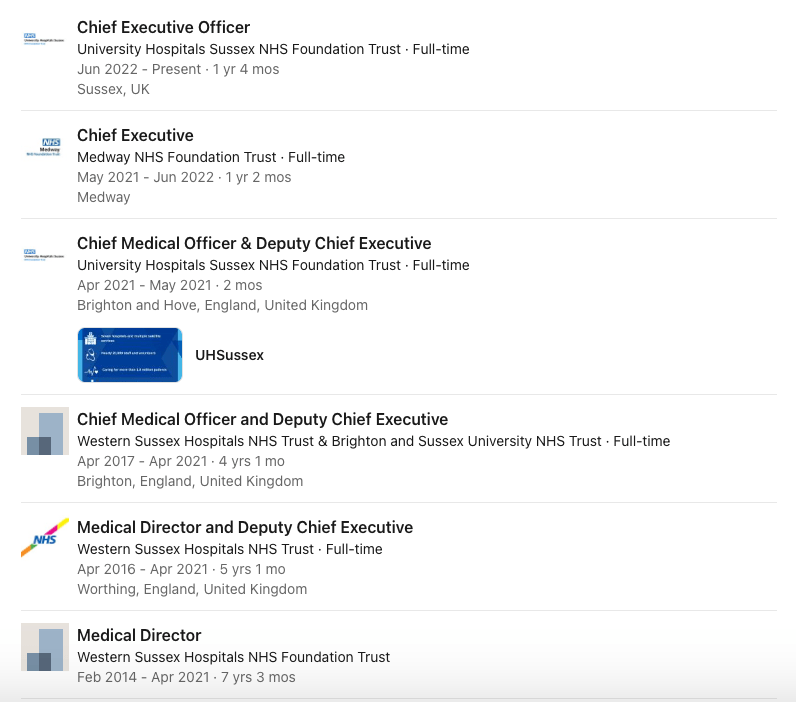
Hunt’s favourites have prospered, including Jackie Daniel the former UHMBT CEO 2012-2018, who was damed and moved onto a plum job at Newcastle.
Daniel was even mentioned favourably at PMQs in a question by the local Tory MP:
“Jackie Daniel received a Damehood for turning around Morecambe Bay Trust, very positive, along with the staff. Would my Rt Hon Friend the Prime Minister, look forward to working with her successor and carry on turning around Morecambe Bay Trust and wish Jackie well.”
In response, Mrs May MP said: “I am happy to join my Hon Friend in paying tribute to the work of the staff at the Morecambe Bay Trust and particularly to wish Dame Jackie well and to recognise and pay tribute to the work she has done turning that trust around.”
Jeremy Hunt et al’s re-branding of Morecambe Bay and a suppressed report on Race concerns
UHMBT has made use of Capsticks’ legal services, including representing the trust against whistleblowers and the drafting of settlement agreements with whistleblowers:
In 2012 UHMBT entered into a highly questionable agreement with a midwife who was accused of cover ups, where redundancy with 14 months pay was agreed on the basis that she would not be investigated for maternity care failures:
“Following discussions between the employee and the trust, the employee has opted to take early redundancy and as a result the employer has agreed not to commence an internal investigation into the employee’s performance as maternity risk manager.”
However, in 2018, it was reported by the Nursing and Midwifery Council that the midwife admitted many of the allegations against her:
“Grace Hansen, acting for the NMC, said: ‘’Jeanette Parkinson was a maternity risk manager at Morecambe Bay Hospitals Trust from 2004 to 2012.
She was also appointed as a supervisor of midwives by the Local Supervising Authority from November 2002.
‘’In 2008 two maternity and three neonatal deaths occurred at Furness General. The charges brought by the NMC relate to Miss Parkinson’s investigation of these these tragic events on behalf of the trust and the LSA.
‘’She has admitted many of the charges and accepts they amount to misconduct and her fitness to practice has been impaired by reasons of that misconduct.
‘’The parties agree the only appropriate and proportionate action is a striking off order. This is the most serious sanction the NMC can impose.”