By Dr Minh Alexander retired consultant psychiatrist
Summary
This post reports on inconsistent information disclosed by CQC on whether or not it has taken regulatory action under CQC Regulation 5 Fit and Proper Persons (FPPR). It also summarises FOI data from the CQC which shows that CQC apparently lacks grip on even the number of NHS FPPR investigations that have taken place. From the data available, only a small proportion of FPPR referrals result in investigations. CQC stated it has accepted all FPPR investigations that it has received, even those which made dubious or frankly perverse findings. The investigations have mostly been conducted by a small pool of external contractors, some of whom have done more than one FPPR investigation. Some contractors have also obtained other employment from the NHS trusts concerned, with questions about potential conflict of interest arising. CQC has refused to disclose the identity of three contractors, making it impossible to know if there were conflicts of interest in their appointment. This confirms the impression of secrecy and unaccountability surrounding the performance management of failing NHS senior managers, and it has serious implications for patient safety. The example of CQC’s dire handling of an FPPR referral on Paula Vennells controversial former Post Office chief executive, who became the Chair of Imperial Healthcare NHS Trust is summarised. The regulator failed to act in a timely manner and then simply shut the referral down after Vennells left the NHS. It failed to examine the trust’s wider leadership and FPPR processes. An Imperial NED had in fact written to me in an attempt to deter me from raising further concerns about Vennells’ suitability. The protection and recycling of wrongdoers continues.
Introduction
My apologies for this late post due to personal circumstances. The post is a summation of the latest information on the Care Quality Commission’s handling of the Fit and Proper Person test in the NHS.
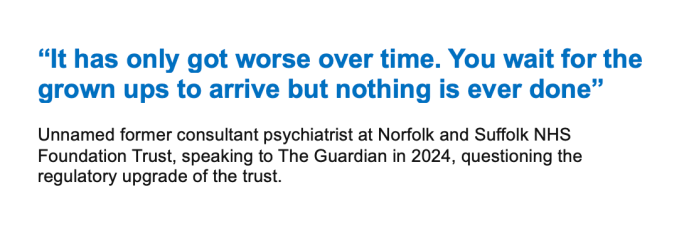
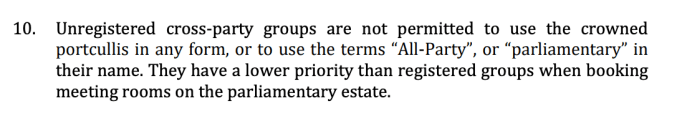
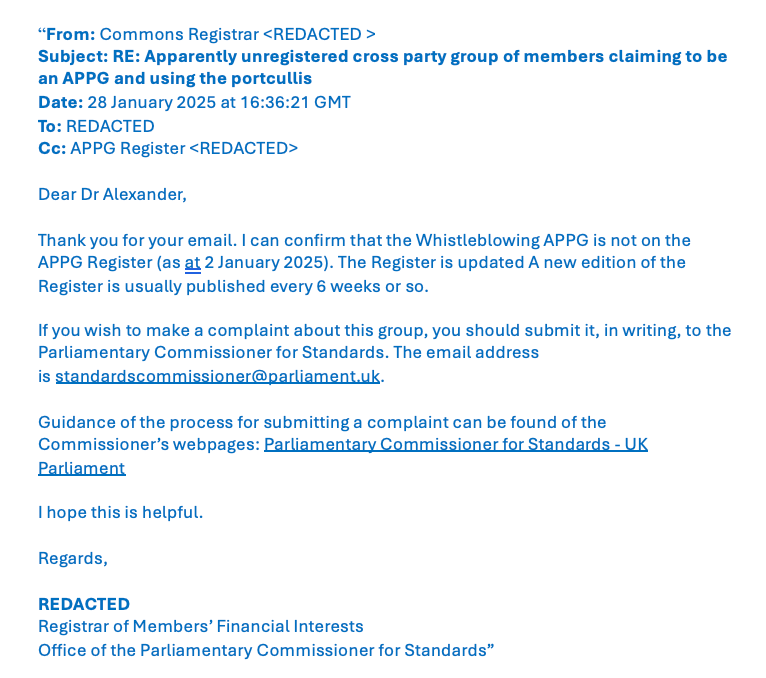
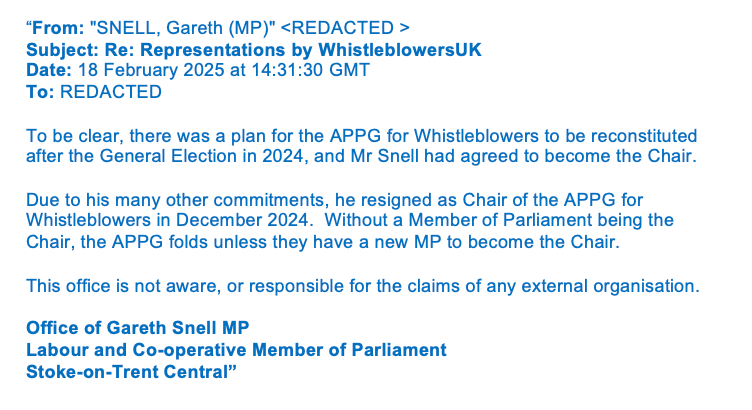
The CQC has a poor reputation, arising in part from lack of distance between the regulator and regulated, and a revolving door between these organisations. This poor reputation includes repeated failures to enforce the 2014 CQC Regulation 5, Fit and Proper Persons which applies to NHS trust directors. It appears that almost no amount of senior management misfeasance results in overt CQC action under the regulation. I say “overt” as there has reportedly been regulatory action which CQC seems to have kept hidden from the public.
CQC’s tortuous acrobatics to avoid holding NHS trust boards to account include the regulator’s claims that it only regulates organisations’ FPPR process and not the fitness of individual directors. When the opposite suits, CQC has claimed that because some trust directors have moved on, there are no grounds to apply FPPR or to examine an organisation’s processes.
In an FOI disclosure of May 2022 CQC admitted that no NHS FPPR processes, since Regulation 5 was introduced in 2014, had led to a finding by CQC’s FPPR panel that any NHS trust was non-compliant with Regulation 5. CQC claimed that this might be due to referred directors leaving or being dismissed.
“…no FPPR referrals relating to NHS trusts have reached an outcome that the provider is noncompliant with the regulation at the conclusion of the panel process…”
This appeared to contradict CQC’s claims to parliament in 2021 that it had taken regulatory action against some NHS trusts under FPPR.
I had also previously found evidence of CQC regulatory action under FPPR at the acute NHS trust in Kettering, which the regulator had not transparently shared with the public.
The reason for the inconsistent information about regulatory action by CQC is not yet clear.
In a curious situation at University Hospitals Leicester NHS Trust, NHS England referred two former NHS trust directors after a financial scandal, only for these referrals to be rejected by CQC on the grounds that former directors did not fall under Regulation 5. Thus, a veil may be drawn over any system failings, no matter how serious.
Paula Vennells’ FPPR referral
A notable example of CQC’s behaviour is that of Paula Vennells the much-criticised former Chief Executive of the Post Office. Vennells is a key figure in the mass miscarriages of justice against innocent sub postmasters who were unsafely convicted of fraud due to Post Office computer errors, which were in fact known to the Post Office. The unsafe convictions started before Vennells joined the Post Office but continued during her tenure, both as group network director and later as CEO. Vennells left the Post Office during legal action by postmasters which was eventually successful. The Post Office resisted throughout and was excoriated by the judge for its disreputable conduct and the unreliable evidence of the Post Office’s senior managers. The subsequent and ongoing public inquiry into the scandal has yielded a wealth of damning evidence all the way up to ministerial level, of wilful blindness and collusion.
Despite the morass at the Post Office, Vennells had a soft landing after her departure from the Post Office, and took up other senior management posts including the Chair of Imperial Healthcare NHS Trust. Unusually, Dido Harding the Chair of NHS Improvement was involved in the appointment at Imperial,
taking part in the selection process. I subsequently referred Vennells to the CQC under Regulation 5 FPPR in December 2019, after the Post Office trial had ended with severe criticism by the High Court of the Post Office’s actions and omissions. Aside from the Post Office’s dissembling about the Horizon computer fiasco, the Court scrutinised the contractual relationship between the Post Office and post masters, and concluded that the Post Office behaved like a “Victorian factory owner”. This is surely a harmful culture that should not be exported into the NHS.
The CQC dragged its feet and no external FPPR investigation took place, albeit one of Imperial’s directors claimed that one had been planned. Sixteen months after my FPPR referral, CQC wrote to say that it was shutting the case down because of Vennell’s departure from Imperial. That is to say, CQC implied that FPPR revolved around an individual and not an organisation’s processes, despite its many previous claims to the contrary.
There was in fact reason to question Imperial’s FPPR process. Disclosed correspondence showed that Vennells took part in constructing comms material in response to a challenge from the public about her fitness.
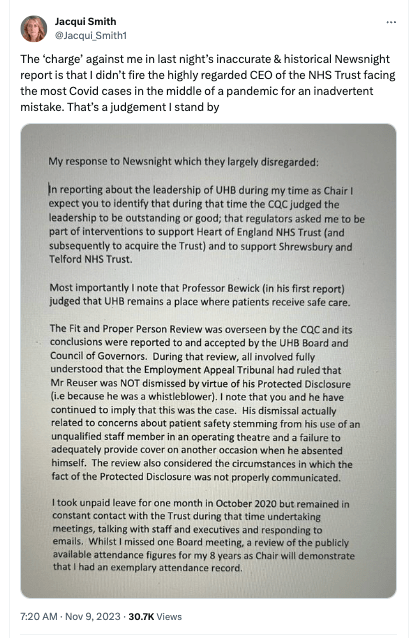
An Imperial non executive also wrote to me characterising my opposition to Vennells’ appointment as a “vendetta”, as later reported by the media in January 2024.
The Imperial NED posited that Vennells might be a victim of misinformation and suggested that my opposition might “backfire” on me in some unspecified manner. The NED claimed that Imperial had given Vennells’ fitness much consideration, and he also implied that the CQC had triggered an external FPPR process:
“I can tell you privately that we have looked again and again at this issue and, as you have acknowledged, we have now agreed to bring in an external assessor to assure us, and the public, that we have shown due diligence”.
He also suggested that no action should be taken until the public inquiry had made a definitive finding about Vennells’ culpability in the Post Office affair:
“It may well be that both the new inquiries, like the past one, find no reason to chastise Paula. It might be that Fujitsu lied or withheld evidence such that her conduct was reasonable. It might that she had too much faith in British justice and in the jury system and believed that, if people had been found guilty, they were probably guilty. It might be that she was cloth eared and should have acted sooner on other evidence. It might be that she listened too intently to lawyers including (I have no doubt) those foolishly advising her to say as little as possible. Or it might be that be that she was significantly culpable, reckless, or even cynical in allowing people to lose their jobs and go to prison for the betterment of the Post Office. When we know, it will be time to act.”
It seems disturbing that thousands of patients’ and trust staff’s interests may be given lower priority than the interests of a former chief executive of a clearly failed organisation, with clear findings by the High Court. Potential patient safety risk should surely not be parked for several years whilst the interests of senior executives are protected. Who wants a director with a history of minimising bad news in a safety critical sector?
Indeed, the fact that the CQC had reportedly negotiated for an external FPPR investigation suggests that the regulator had not originally planned to defer the FPPR process until after the Post Office public inquiry, despite the Imperial NED’s assertions that no action should be taken until the public inquiry’s determinations about Vennells had concluded.
The attitude of the Imperial trust board suggests that Trust process and not just Vennell’s personal fitness was relevant to the FPPR, but it was never examined.
CQC FOI disclosures on the conduct of Regulation 5 FPPR
On 11 October 2023 and 29 November 2023 the CQC responded to FOI requests on its handling of Regulation 5 FPPR as follows:
Since 2014 CQC has received “153 referrals from trusts involving 223 directors who may have been referred once or more.”
CQC’s FPPR panel (usually chaired by the Chief Inspector of Hospitals or a deputy) had “ followed up on 96 referrals.”
Astonishingly, CQC said it did not know how many of the referrals had led to an investigation:“We don’t hold this information.”
CQC disclosed that it had received FPPR investigation reports on only a small proportion of the referrals:“We have received 30 investigation reports”
Three of these thirty investigations had been conducted internally:
“We don’t hold information on how many FPPR investigations were conducted internally. We have received 3 reports from internal reviews/investigations.”
Independent investigation reports were received in 27 of the 30 cases:
“We have received 27 reports from external independent investigations.”
When questioned about the low number of external independent investigations and asked how it satisfied itself that Regulation 5 had been met in all cases CQC replied:
“The CQC received information from the trusts that either gives assurance for regulation 5 on each of its directors or confirms what the trust is doing to ensure the regulation is being met. There are referrals recorded where directors have left the NHS during the process which would not have resulted in an investigation or report.”
CQC had not rejected any of the FPPR investigation reports:
“Question
By rejected, I mean “Did CQC find the reports to be unacceptable in nature or quality?”
For example, were any of the reports so unacceptable that CQC therefore asked for further reports or re-investigation and/or revision of some aspect of the reports?”
Answer
CQC has not rejected a report in the manor [sic] which you describe.”
Given some of the outcomes of the FPPR investigations, some sharply contradicting evidenced, legal determinations by Employment Tribunals, this too is astonishing.
These 27 investigation reports had been carried out by a small pool of external investigators:
“The number of external contractors is 17. Some contractors have been used more than once.”
CQC listed the contractors used for these external FPPR investigations thus:
Tamarix People
Fiona Scolding QC
Unique Health Solutions
Law2Business
Serjeants Inn Chambers / Clyde & Co
Mark Sutton QC
Bevan Brittan
Deloitte
Cordis Bright Consulting
YSC – Young Samuel Chambers
Good Governance Institute
Capsticks Solicitors
Ibex Gale
EY
3 Independent Individuals
In an FOI response of 20 November 2023, CQC later disclosed information on how many investigations had been conducted by each of these contractors:
Fiona Scolding KC (2)
Unique Health Solutions (2)
Law2Business (1)
Serjeants Inn Chambers / Clyde & Co (1)
Mark Sutton KC (1)
Bevan Brittan (1)
Deloitte (2)
Cordis Bright Consulting (1)
YSC – Young Samuel Chambers (1) Good Governance Institute (1)
Capsticks Solicitors (3)
Ibex Gale (2)
EY (1)
3 Independent Individuals (3)
CQC declined to disclose the identity of the three independent individuals. Interestingly, CQC justified this by asserting that barristers might expect their identities to be disclosed but that non barristers might not.
It is therefore not possible to tell if conflicts of interest surround the hiring of the three unnamed, allegedly independent individuals on CQC’s list of external contractors.
CQC refused to disclose to which NHS trusts the 30 investigations related, further obscuring any possible conflicts of interest.
But CQC admitted that the regulator itself had previously purchased services from Deloitte and EY.
There are some interconnections with NHS whistleblower cases.
CQC disclosed that the FPPR investigation on Portsmouth medical director John Knighton was conducted by Mark Sutton KC. I referred John Knighton because of his mistreatment and unfair dismissal of Dr Jasna Macanovic, Portsmouth whistleblower, as determined by an Employment Tribunal. CQC found no breach of FPPR and Knighton remains as medical director.
Of note, Mark Sutton received further employment by Portsmouth and he later represented the trust at Dr Macanovic’s employment tribunal remedy hearing. At the Tribunal hearing, which I observed, the Tribunal criticised the Trust for attempts to shift blame (and by implication, reduce liability).
Mark Sutton also represented Hampshire Hospitals in the Employment Tribunal case of Mr Martyn Pitman, Obstetric whistleblower.
Furthermore, Law2Business is on the list of contractors who have carried out FPPR investigations. This company was owned by a Portsmouth Non Executive Director who conducted a whistleblowing investigation at Hampshire Hospitals into Martyn Pitman’s case. Mr Pitman contended that the investigation was flawed and links between the two trusts were noted. CQC denied that Law2Business had carried out any FPPR investigations at Portsmouth or Hampshire.
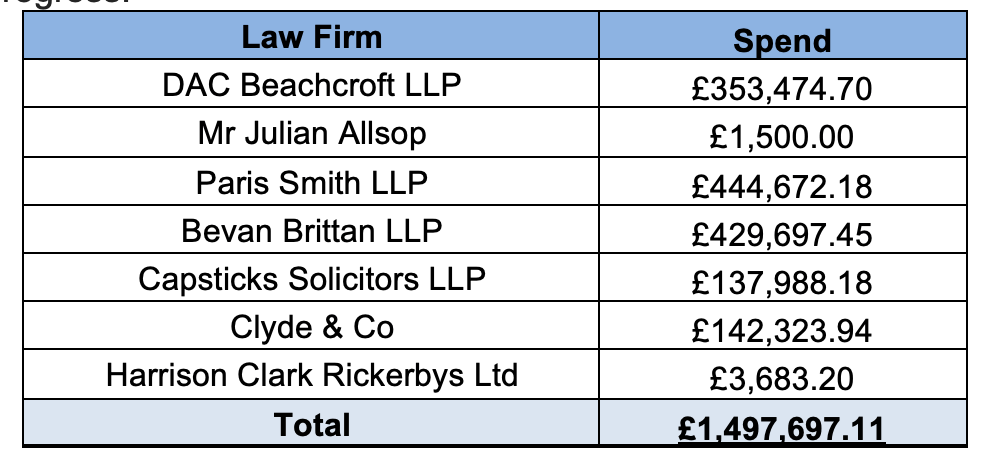
Concerning the law firm Bevan Brittan, which appears on CQC’s list, this may relate to the FPPR investigation of David Rosser former medical director and then CEO of University Hospitals Birmingham NHS Foundation Trust. In this matter, the CQC wrongly claimed to me that an independent investigation had taken place, when it was an internally led investigation by a trust employee. The investigation had contributions from Bevan Brittan, which was a firm retained by the trust and had received half a million pounds from the trust in the three years before the FPPR investigation. The finding that there was no breach of Regulation 5 seems astounding given the seriousness of the Employment Tribunal’s criticism of Rosser.
With respect to the contractor Tamarix People, which has according to CQC conducted four NHS FPPR investigations, this one-woman company was previously engaged to investigate conflict between Trust Directors at Wirral.
Regarding the Countess of Chester Hospital NHS Trust, where the Letby killings took place and continued after clinical staff raised concerns, CQC declined to say if there is a current FPPR process:
“CQC cannot currently comment on any FPPR referrals that we may have received subsequent to the criminal conviction of Lucy Letby.
We consider this information – including confirming whether or not CQC has received referrals – to be exempt from disclosure under section 31 of FOIA (law enforcement / prejudice to regulatory functions).
We recognise the public interest in transparency on this matter but consider that there is an overriding public interest in prevention of any prejudice.”
These are the two most recent CQC FOIA disclosures about FPPR:
CQC FOI response on FPPR CQC IAT 2324 0556 11 October 2023
CQC FOI response on FPP CQC IAT 2324 0690 29 November 2023
In short, there is limited transparency on how NHS trusts and the CQC handle Regulation 5 FPPR, even allowing for legitimate considerations of privacy. Indeed, the public interest test under FOIA should be weighted differently for the directors of NHS trusts, who handle budgets of hundreds of millions and who hold the safety of patients in their hands
Only a small proportion of FPPR referrals result in an investigation, and where the investigations are contracted out, they are given to a small pool of investigators, some of whom may provide other services to the relevant NHS trust.
There is a potential for pro-employer bias, in what are matters of huge public interest.
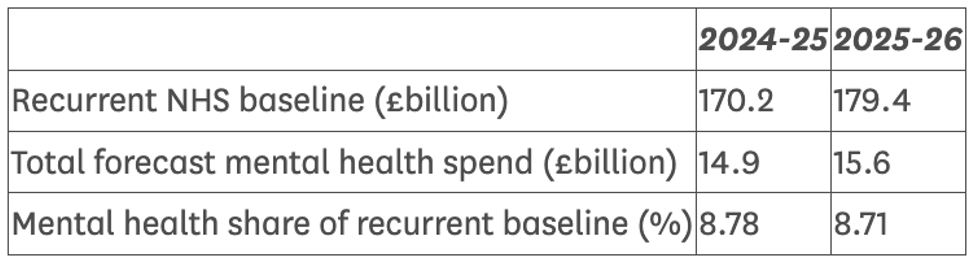
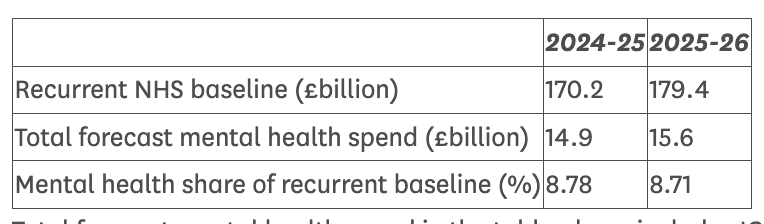
The waste of public money in servicing ineffective, secretive and half-hearted enforcement of Regulation 5 is lamentable.
The greatest cost is to NHS safety culture and patients’ interests.
Many NHS senior managers continue to protect their own positions.
The annual NHS staff survey report was published yesterday, with a low response rate of 47%. It nevertheless shows that roughly a third of NHS staff still do not feel safe to speak up, and about half do not think concerns would be acted on.
Personal update
I have been unwell and also much occupied with family responsibilities. For a period, I will not be able to do as much campaign work as usual. I may not be able to respond to all messages, but I appreciate the support and concern that many have shown. I hope to resume more work at some point.
RELATED ITEMS
Sorry is the hardest word: CQC, Paula Vasco-Knight and Regulation 5 Fit and Proper Persons
Mr Tristan Reuser’s whistleblowing case: Scandalous employer and regulatory behaviour on FPPR
Mr Shyam Kumar, Surgeon and vindicated NHS whistleblower’s case: CQC sacked a whistleblower for disclosures about its poor regulatory performance, and dug for dirt on the whistleblower