By Dr Minh Alexander retired consultant psychiatrist 30 July 2022
Earlier this month I submitted evidence to parliament via Public Accounts Committee (PAC), one of the more rigorous committees in holding the Care Quality Commission to account.
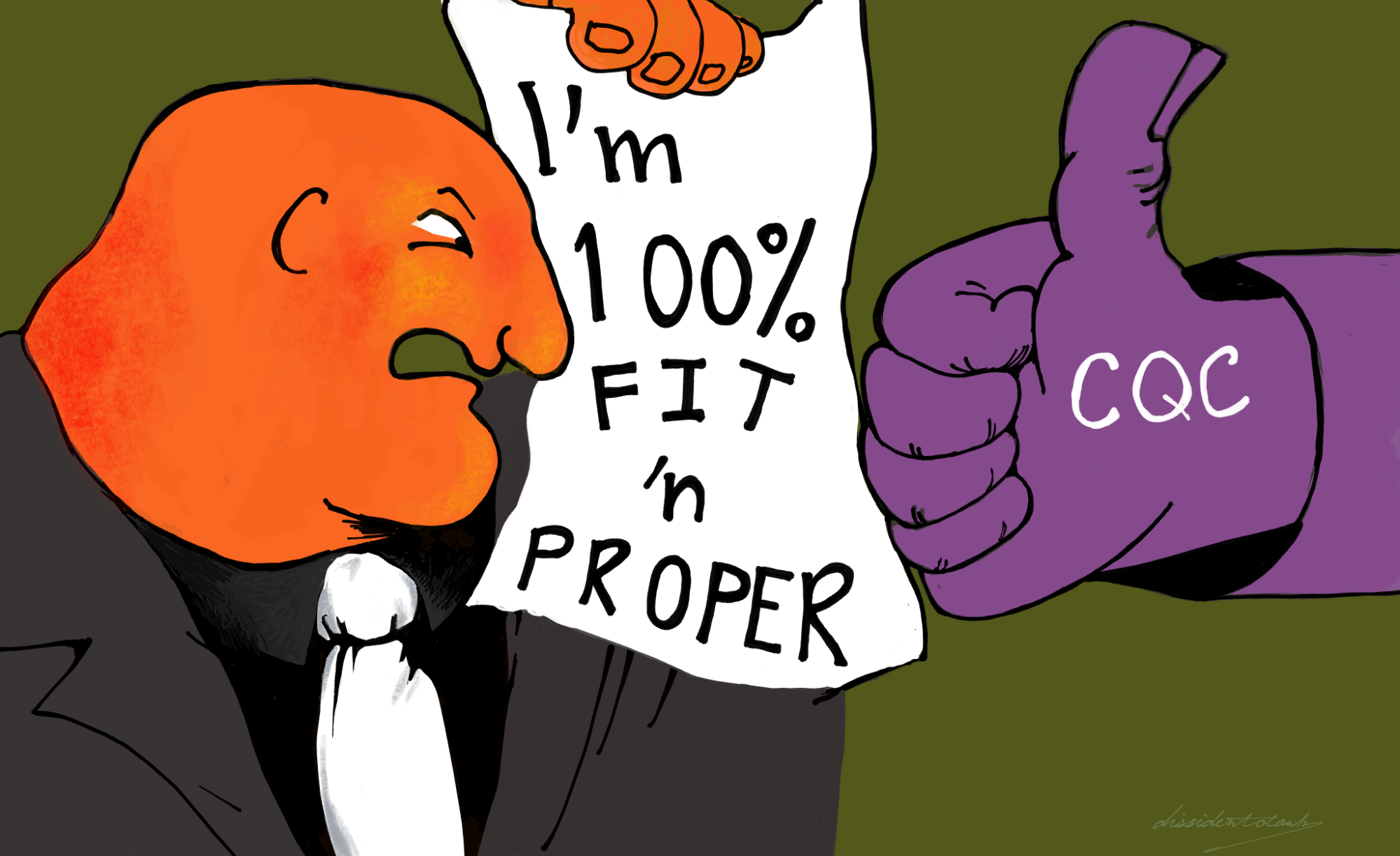
I asked PAC to consider CQC’s track record of failure in the last eight years to properly apply Regulation 5 Fit and Proper Persons (FPPR). This is supposed to ensure that service providers have suitable directors who have not been guilty of or privy to serious misconduct or mismanagement.
Unsurprisingly, it was recently confirmed by FOI that CQC has NEVER found any NHS trust to be in breach of FPPR.
Unusually, the Committee has advised that it has passed the evidence to the National Audit Office, “who may be able to look into your [my] concerns”.
I have no idea if anything will come of this.
The NAO does solid work most of the time, but it had a touch of the vapours when dealing with an issue of whistleblowing policy and the CQC some years ago. It examined itself and the CQC amongst some other bodies, as examples of Prescribed Persons under our woeful whistleblowing legislation, and came to some surprisingly sunny conclusions.
Prescribed Persons or the Pretence of PIDA: How UK Whistleblowers are Ignored
We shall see.
In the meantime, the correspondence exchange with PAC is provided below.
CORRESPONDENCE WITH PUBLIC ACCOUNTS COMMITTEE
—–Original Message—–
From: NATHOO, Heather <REDACTED>
To: Minh Alexander <REDACTED>
Sent: Thu, 21 Jul 2022 12:10
Subject: RE: Almost non-existent regulation of failing NHS managers is still the norm – gagging
Dear Dr Alexander
Thank you for your email to the Public Accounts Committee and for sharing the information below. I have forwarded this to my colleagues at the National Audit Office who will be able to look into the details of your concerns. They will be in touch if they have any questions.
If the PAC have any upcoming inquiries related to CQC then there is also the opportunity to submit written evidence. Evidence can be submitted anonymously.
The committee is currently agreeing on its future programme. Whilst I am not aware of any plans to look into the CQC in the near future, our website will be kept up to date so it’s worth checking intermittently to see what we have open.
Thank you again for writing to the PAC, and all the best
Heather
Heather Nathoo
Chair LiaisonPublic Accounts Committee
From: Minh Alexander
Subject: Re: Almost non-existent regulation of failing NHS managers is still the norm – gagging
Date: 5 July 2022 at 18:07:17 BST
To: [Public Accounts Committee and others, email addresses redacted]
BY EMAIL
Dame Meg Hillier MP and Public Accounts Committee colleagues
Health and Social Care Committee
5 July 2022
Dear Dame Meg and colleagues,
Re: Almost non-existent regulation of failing NHS managers is still the norm – gagging
Further to my letter on this subject yesterday, I forward a just published article by The Independent as additional evidence.
Patients will suffer as a result of NHS ‘gagging’ clauses, whistleblower warns
This covers an important additional detail in the case of whistleblower surgeon Mr Tristan Reuser.
His trust, University Hospitals Birmingham NHS Foundation Trust tried to settle with him in the latter stages of the Employment Tribunal litigation. The trust explicitly sought to gag him and to arrange settlement entirely outside of the ET process.
The effect of this would have been to conceal the damning reasons issued by the ET for its cost order against the trust, in which it criticised the trust severely for failure to disclose documents, from which the ET could not rule out “deliberate dishonesty”.
Settlement was not reached but the trust was reportedly willing to pay almost £100K for silence, which in the circumstances seems a serious misuse of public funds.
There has been no accountable [sic] for this conduct by trust managers, illustrating the general point that regulation of failing NHS managers is still almost non existent.
Yours sincerely,
Dr Minh Alexander
—–Original Message—–
From: Minh Alexander
To: [Public Accounts Committee and others, email addresses redacted]
Sent: Mon, 4 Jul 2022 15:13
Subject: Re: Almost non-existent regulation of failing NHS managers is still the norm
BY EMAIL
Dame Meg Hillier MP and Public Accounts Committee colleagues
Health and Social Care Committee
4 July 2022
Dear Dame Meg and colleagues,
Re: Almost non-existent regulation of failing NHS managers is still the norm
I write to raise a serious concern that the Care Quality Commission and others are continuing to fail to protect the public and NHS staff from failing NHS managers.
As far as I can see, there has been no real learning from the MidStaffs disaster or the related public inquiry which concluded that a key contributory factor was serious failure by the trust board.
CQC AND REGULATION 5 FIT AND PROPER PERSONS
The government has gone through the motions of enacting a recommendation of the 2013 MidStaffs Public Inquiry report by amending the CQC’s regulations in 2014 and giving the CQC the responsibility of regulating whether service providers have Fit and Proper directors.
However, the CQC has now admitted that it has NEVER found any NHS trust to be in breach of CQC Regulation 5 Fit and Proper Persons since 2014:
CQC FOI disclosure 25 May 2022 FPPR Fit and Proper Persons
CQC weakly contends that it might have done, had some individuals not resigned or been sacked before the FPPR process concluded.
However, as CQC has not ever breached any trusts even in the face of gross evidence of unethical conduct, such as Employment Tribunal-tested evidence of whistleblower reprisal or being party to manipulation of evidence, it is arguable as to whether CQC’s contention is credible.
CQC has claimed on many occasions to the public (patients, families and whistleblowers) that it has no responsibility for determining whether providers’ directors are Fit and Proper Persons.
It has instead typically claimed that its remit is limited to regulating the soundness of providers’ processes for ensuring their directors’ fitness.
Usually, the CQC gives no account of how it achieves this. Referrers are faced with a black box into which they insert a referral, from which they then receive the briefest of letters from the CQC telling them that the regulator has been satisfied that the providers’ process is satisfactory and that there is no breach of Regulation 5.
Very seriously, I discovered that the CQC failed even to ensure a sound FPPR process with any diligence. This arose from an FPPR process concerning the CEO of University Hospitals Birmingham NHS Foundation Trust. I asked for confirmation that the CQC had reviewed original assurance documents, as some parties were concerned that this had not happened. In replying to me, the CQC misled me by claiming that an “independent” FPPR review had been arranged by the trust.
This was untrue. It became evident that a subordinate trust employee and a lawyer from a firm previously retained by the trust, which had undertaken almost £500K worth of work for the trust in the previous three years, had conducted the FPPR review.
A trust non executive director who had been a party to related
disciplinary processes criticised by an Employment Tribunal was also involved in the FPPR review, creating another conflict of interest.
The details of the matter can be found here:
It now appears that the same retained law firm also conducted a previous FPPR review for the trust, which may have been an FPPR review on the same director. I am waiting for the trust’s clarification.
A question arises of how many times has the CQC accepted such compromised FPPR evidence?
The CQC dug itself in deeper by claiming that it had no say over how trusts conducted FPPR reviews, despite its published and internal material making it plain that its regulatory process includes assessing whether providers have “robust” FPPR process.
As a late development in the case, the Employment Tribunal published reasons for a cost order issued against University Hospitals Birmingham NHS Foundation Trust on 5 May 2022, which were damning:
ET reasons to award costs against University Hospitals Birmingham NHS Foundation Trust
There were serious criticisms of the trust for failures to disclose highly relevant documents either to the Tribunal or to the whistleblower Mr Tristan Reuser surgeon under GDPR. The Tribunal concluded that it could not rule out “deliberate dishonesty” by the trust and also observed that it considered that there could be future failings of governance by the trust.
I sent the above ET reasons document to Rosie Benneyworth the CQC Chief Inspector for Primary Care and current Chair of CQCs FPPR panel. She did not respond.
The truth is that the CQC admitted to whistleblowers in 2014, and again in its internal guidance to its own staff, that:
1) CQC can make a determination of whether providers directors are unfit, if it so wishes
2) CQC does not have direct powers to remove an unfit director, but can indirectly pressure a provider to remove an unfit director by using other powers
“It is not the responsibility of CQC to ensure fitness although we can take action against the provider if we believe an unfit person to be in a directorship position.”
The internal CQC guidance which makes this clear can be found here:
It appears that CQC simply does not have either the political will or the permission to act.
Disclosed correspondence of 4 May 2022 from the CQC to the Health Secretary about CQC’s failures in regulating maternity safety at Shrewsbury and Telford Hospital NHS Trust, reveals renewed CQC promises that the organisation has purportedly – yet again – revamped its processes:
CQC letter 4 May 2022 to DHSC re maternity safety and Ockenden report
Amongst these is a claim of September 2021 that CQC will regulate leadership more effectively in the future.
“…We’ll work with others to develop solutions to ensure that all services have support and leadership…”
This seems an empty claim when set against the reality of how CQC actually responds when asked to take action under Regulation 5 Fit and Proper Persons.
NHSENGLAND/IMPROVEMENT, DHSC AND THE KARK REVIEW
As a result of concerns about the disappointing lack of action under Regulation 5 Fit and Proper Persons and in view of very similar governance failures at Liverpool Community Health NHS Trust as were seen at MidStaffs, the government in 2018 commissioned the Kark Review on addressing failures of NHS management:
Kark Review Fit and Proper Persons in the NHS
The review stopped short of recommending full regulation for NHS managers but it did consider a range of structured measures, including creation of a database to help track findings of misconduct and unethical behaviour, and a disbarring mechanism.
This too has simply not been acted upon.
NHS England/Improvement set up a steering group – the so called Kark Reference Group – but this was not transparent and minutes were not public. The majority of the minutes remain withheld.
A recent meeting with NHSE/I revealed that the NHS was still waiting for permission from Ministers to implement the Kark review recommendations in some form:
Minutes of telephone meeting with NHSE/I 18 May 2022
It is not even clear if a Kark register on NHS managers, if approved, will be retroactive. So it is possible that the longer the delay in implementation drags on, the more historical misconduct will be omitted from any register that is eventually set up.
NHS whistleblowers continue to be seriously harmed all the time.
Some of these whistleblowers are falsely promised that CQC will protect them and will hold erring NHS directors to account with Regulation 5. I have recently seen text correspondence from the CQC to this effect. The reality is the opposite.
A cabal of senior NHS managers, operating through a revolving door between providers and regulators, and sometimes the Department of Health and Social Care, more often than not acts with impunity. Failure is rewarded, cronyism and cover ups are the norm, faux governance and questionable investigations are arranged time and again, thus wasting public money to protect senior individuals’ reputations.
Only today, I received news that NHS England/Improvement is proposing effectively to investigate itself in an extremely serious matter of covered up deaths, exposed by whistleblowers who made futile attempts to seek help from NHSE/I.
This self-serving behaviour and impunity contrasts with the arbitrary, harsh discipline that is meted out to frontline staff when it suits abusive managers to do so, in the name of control or cover up. The panoply of abuse includes wholly unnecessary or even malicious suspensions, engineered dismissals through employer-provoked breakdown of relationships and vexatious referrals to professional regulators.
Some NHS boards refuse to accept the enormous impact of their harsh disciplinary actions against frontline staff. The Chair of University Hospitals Birmingham NHS Foundation Trust astonishingly stated in correspondence that GMC referrals should not be seen as punitive, despite the well-publicised deaths of and illness in doctors who are referred.
This is all the more remarkable because this trust admitted that of 26 GMC referrals made by the trust over a ten year period, none resulted in any further action against the referred doctors by the GMC. This raised questions about the quality of this trust’s referrals and whether the trust referred the right doctors.
UHB FOI disclosure April 2022 GMC referrals
The failure by the government and the NHS to act on NAO 2003 recommendations to track NHS staff suspensions rather says it all about poor NHS managers being allowed to flourish:
This normalised abuse represents an unaffordable waste of precious and very expensively trained and developed personnel, especially at a time when the workforce has been strained and depleted by the pandemic and socioeconomic factors.
We also see the cost, human and economic, in the continuing trail of NHS-related public inquiries and external reviews into serious care failings.
The prospect of being referred to a professional regulator is something that does not currently constrain NHS managers.
If it were, this might perhaps inject more accountability to the public, as opposed to the downwards pressure from the Department of Health and Social Care that has so often been identified as an unhelpful factor in care failings.
REQUEST
I would be very grateful if PAC could turn its attention to the poor regulation of failing NHS managers, and in particular the CQC’s poor performance, NHSE’I’s failure to implement the Kark review and the DHSC’s reported failure to give NHSE/I permission to implement Kark.
I would also be grateful if PAC and HSCC would take this evidence submission into account whenever they next hold their respective CQC accountability hearings.
Yours sincerely,
Dr Minh Alexander
Retired consultant psychiatrist and NHS whistleblower
PETITION
Please click and add your signature to this petition to reform UK whistleblowing law – whistleblowers protect us all but weak UK law leaves them wholly exposed and it is a threat to public safety
Replace weak UK whistleblowing law and protect whistleblowers and the public
RELATED ITEMS
Is there a ‘club culture’ at the heart of the NHS’s quality regulator?
Whistleblowers have continued to emerge at UHB:
Multiple whistleblowers flag ‘heartbreaking’ incidents at major trust

A FIFTH never event of the wrong type of blood given has just been reported at UHB:
Major trust records fifth never event at troubled department
University Hospitals Birmingham NHS Foundation Trust also made the headlines on 5 June 2022 because of reportedly poor treatment of doctors in training in obstetrics and gynaecology, requiring regulatory intervention:
Trainee doctors in ‘meltdown’ at major hospital maternity department
Based on Tristan Reuser’s case and others, NHS Resolution agreed that NCAS’ successor body will consider safeguards against being fed false information by unscrupulous employers:

In true NHS musical chairs style, it was announced on 7 June 2022 that Rosie Benneyworth current chair of the CQC FPPR panel is being posted to HSIB:

Dr Rosie Benneyworth appointed interim Chief Investigator
“We know that most people get good care in the NHS, but sometimes they don’t get the outcomes they need or things go wrong. In these circumstances, it is vital that as a system we reflect and learn from these events to improve the safety of care”
“Rosie takes up her post with HSIB on 1 August 2022.”
Let us hope that Benneyworth does not take to tearing up any rule books at HSIB.
A particularly gross example of CQC conflict of interest and failure on FPPR was when it passed its notorious former Chair Jo Williams as a Fit and Proper Person, removing obstacles to her recycling back into the NHS fold:
Jane Archibald’s shocking whistleblowing case about a cover up of an unqualified assistant being allowed to run epilepsy clinics and vary complex epilepsy medication featured a failure by her former CEO Stephen Eames to respond to her disclosures. He simply did not respond to her correspondence. NHSE/I has been asked to review his suitability for his current post as CEO of the Humber region ICS.
Dr Jasna Macanovic’s recent NHS whistleblowing case adds to the pile of managerial recycling scandals. John Knighton the medical director found by the ET to be centrally involved in her premeditated unfair dismissal has been protected by the trust and Mark Cubbon the trust CEO who failed to ensure her protection as a whistleblower has been promoted to a senior post at NHS England.
An FPPR referral has now been made arising from the executive failures in this matter.
The Flexible CQC, FPPR & Kettering General Hospital NHS Foundation Trust\
Sorry is the hardest word: CQC, Paula Vasco-Knight and Regulation 5 Fit and Proper Persons
Steve Trenchard, NHS regulators & FPPR
FPPR: CQC has lost all moral authority, but what will the National Guardian do?
Postscripts on Paula. NHS England’s apologia & regulatory reticence

Thank you for your report, Dr A.
Even with the aid of a toothy smiling face and a cartoon, I am shocked by the lack of enthusiasm of certain NHS personnel for being held accountable for their actions. Plus, an absence of concern for the resulting harm to the innocent. That tells its own story.
What a dismal word salad of excuses from regulators.
How depressing. And how predictable.
LikeLike