Dr Minh Alexander retired consultant psychiatrist 26 July 2023
| Summary: After a delay and only as a result of intervention from the ICO, the GMC has disclosed information on its processes which shows that it is not centrally collating data to track variations between employers who refer doctors to the GMC. It has not followed up many cases where employer referrals have not even led to an investigation by the GMC, by feeding back to the relevant employers. This is despite a claim that it is GMC procedure to do so. GMC’s policy does not cover feedback to employers after cases which are investigated but result in no further action, which seems an omission. Although the GMC advises that it works with employers to reduce the level of unnecessary referrals, it does not keep a record of whether referrals are necessary. The GMC declines to tighten its rules to deter medical managers from making vexatious referrals. The GMC has also finally broken its silence about referrals by University Hospitals Birmingham NHS Foundation Trust. According to the GMC, even “corrected” data by the trust contained inaccuracies, but a broad picture of a high proportion of referrals leading to no investigation or to no further action by the GMC is confirmed. It is hard to see how GMC is safeguarding whistleblowers effectively given the above omissions. |
The General Medical Council is the professional regulator for doctors and is funded by compulsory fees paid by doctors.
It has lost the confidence of many doctors after years of poor decisions, including the harmful handling of cases and related suicides of referred doctors, inconsistent approaches and perceived unfairness towards of ethnic minorities, caprice in both excessive harshness and leniency, failure to protect the public from doctors such as Ian Paterson the jailed breast surgeon whilst allowing employers to harm whistleblowers and latterly, and latterly failure to take action in cases of vaccine disinformation by a few individuals.
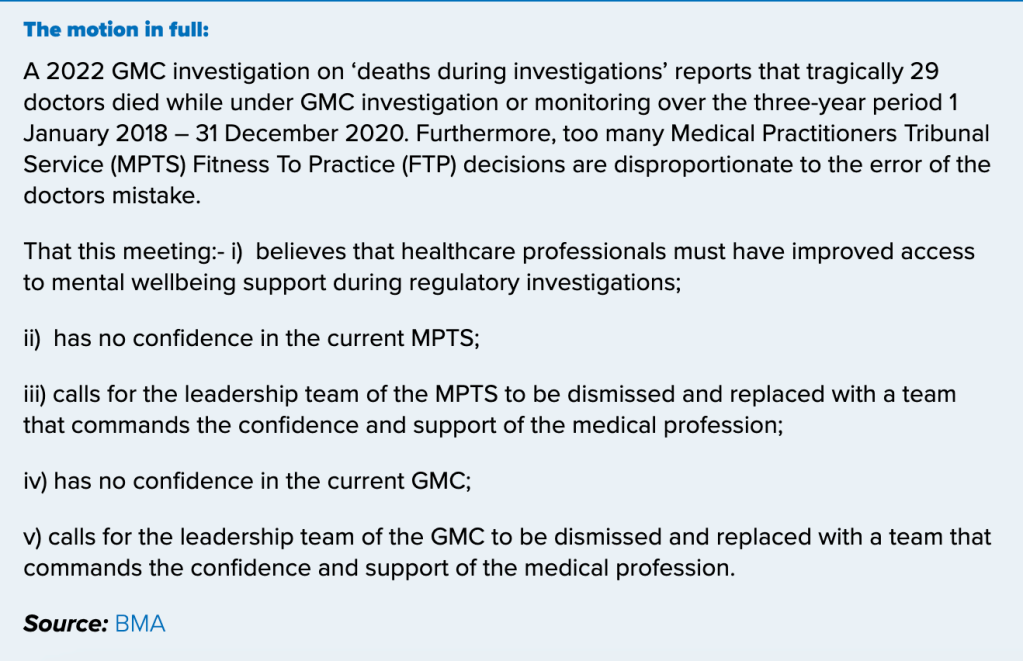
At the recent annual BMA conference, a motion of no confidence in the GMC passed. This included a call for senior officers of the GMC and Medical Practitioners Tribunal Service to be dismissed.BMA declares it has no confidence in the GMC 4 July 2023
The GMC’s handling of whistleblowing cases was reviewed in 2015 by former Court of Appeal judge Tony Hooper, with recommendations adopted to safeguard whistleblowers.
Arising from this, the GMC reviewed the fitness of David Rosser medical director at University Hospitals Birmingham NHS Foundation Trust who had referred Mr Tristan Reuser a whistleblower but falsely declared that the referred doctor had NOT made public interest disclosures.
Last year, UHB supplied flawed data about its GMC referrals. It was asked to correct these when it became clear from published MPTS data that the UHB FOI data was flawed. UHB did not correct the data until 13 April 2023:
| RESPONSE BY DAVID BURBRIDGE, UHB CHIEF LEGAL OFFICER, 13 APRIL 2023 Dear Dr Alexander Please find below a response to your email to Dame Yve Buckland, dated 29 March. For the period 1 April 2012 to 31 March 2022: – How many doctors the trust referred to the GMC ? At UHB (prior to and post the merger with Heart of England NHS Foundation Trust (“HEFT”)) there were 22 referrals At HEFT (prior to the merger with UHB) there were 16 (3 of these are dated just after the date of merger 1.4.2018, but are attributed to HEFT – we believe this may be because there was contact before the change of RO) – How many of these referrals were signed off by the medical director? At UHB 14/22, the remainder were signed off by Deputy Medical Director or acting Medical Director At HEFT 6/16 were signed off by the Medical Director and the remainder were by Deputy or Associate Medical Directors. – How many of these referrals resulted in no further action by the GMC? UHB – 4 were concluded at triage, 7 were investigated and concluded with no action, 11 were subject to advice, warning, undertakings, suspension or erasure HEFT – 3 were concluded at triage, 4 were investigated and concluded with no action, 9 were subject to advice, warning, undertakings, suspension or erasure – How many doctors died whilst under GMC investigation or monitoring? None – How many doctors died by suicide whilst under GMC investigation or monitoring? None Regards David Burbridge Chief Legal Officer |
In the months between, the trust and ICB had the gall to spin the supply of false data by UHB as misreporting by BBC Newsnight, who merely reported what the trust had claimed.
On 1 May 2023 I asked the GMC to verify the “corrected” UHB data. I also asked the GMC to demonstrate that it had systems to hold rogue employers who make vexatious referrals to account.
The GMC resisted this FOI despite reminders. I therefore referred this failure to the ICO who ordered the GMC to provide a response.
This is the GMC’s reluctant reply, which came from the Fitness to Practice Policy Enquiries Team:
GMC FOI reply 25 July 2023 After the Hooper report and UHB 24072023
It is a detailed reply, with some claims of good practice, but it is evasive and obfuscatory on important points.
Data about UHB’s referrals to the GMC
The GMC’s response provides the following data on GMC referrals by UHB:
| “With respect to the data that UBH provided, the data on the total number of referrals is correct, however there is an inaccuracy in the data on cases which concluded at triage / concluded with no actions: “UHB reported that of the 22 referrals, four were concluded at triage, seven were investigated and concluded with no action, 11 were subject to advice, warning, undertakings, suspension or erasure. In fact, of the 22 referrals from UHB the outcomes were that three were concluded at triage, eight were investigated and concluded with no action and 11 were subject to advice, warning, undertakings, suspension or erasure. Turning to Heart of England NHS Foundation Trust (HEFT), the data you were provided with states that six of 16 referrals were signed off by the Medical Director and the remainder were by Deputy or Associate Medical Directors. Our data indicates that the number of referrals by the Medical Director was five. Finally, one of the nine referrals which was said to have ended by way of advice, warning, undertakings, suspension or erasure actually ended by means of being referred to the doctor’s Responsible Officer. Further information on outcomes Of the 11 investigations stemming from UHB referrals which were subject to advice, warning, undertakings, suspension or erasure, two were closed with advice. The number for HEFT is also two.” |
GMC’s tracking of the quality of employers’ referrals
The GMC has advised that since May 2022, it has operated a policy of feeding back to employers where referrals do not result in a GMC investigation, but has only provided feedback on three occasions:
“The feedback loop between our Case Examiners and the Employer Liaison Service (ELS) was implemented in May 2022 in response to the following recommendation in Fair to Refer?
Where a referral is received from an employer/provider which does not result in the GMC opening an investigation, the ELA [Employment Liaison Adviser] and RO [Responsible Officer] should have a discussion to identify learning in relation to the original referral. If a referral comes in that either doesn’t involve an ELA, or does involve an ELA but doesn’t get past our initial triage stage, the ELA team scrutinise this to understand what learning can be taken from the referral. For those referrals that get to a CE decision, if the CE [Case Examiner] identifies learning for the referring organisation about the referral, then that is shared back via the ELA.
Providing feedback is at the discretion of the CEs to do so when appropriate. As of May 2023, there had been three cases where it was appropriate to utilise this feedback loop.”
“Triage / RO feedback loop:
we have also implemented a further feedback loop between the team that initially assess concerns (triage) and our ELS to support further discussion between the ELS and ROs on cases that have been considered and closed by us at triage where there are opportunities to feedback on aspects of the referral that would be useful learning for ROs and their organisations.”
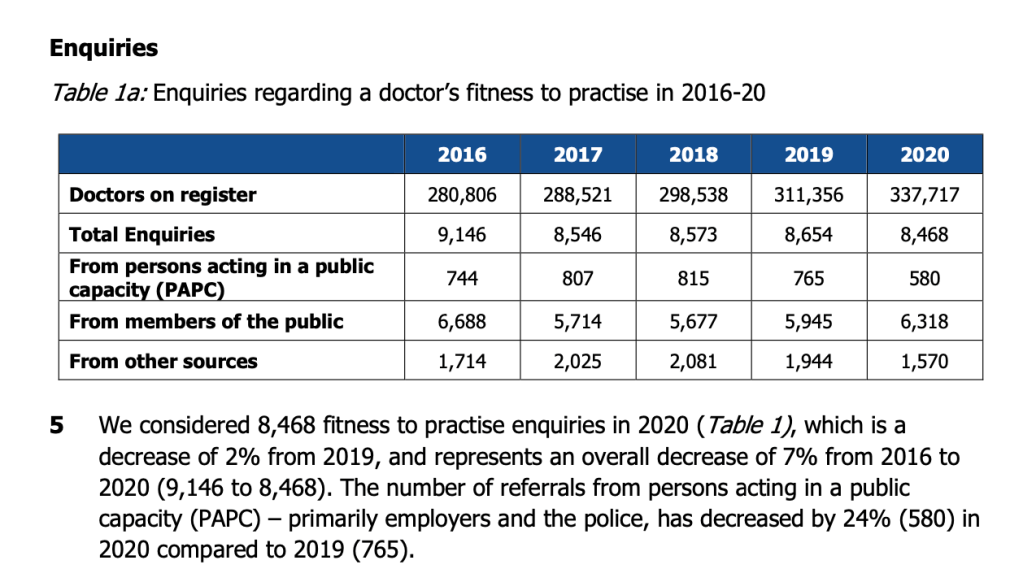
The GMC receives hundreds of referrals from employers each year.
GMC has indicated in its FOI response that 85% of these referrals from employers pass the threshold for investigation:
“85% of the referrals we received from ROs [Responsible Officers] in 2022 met our test for an investigation.”
It seems anomalous that the GMC has given feedback to employers on only three occasions since May 2022.
It is also a concern that GMC appears not to be concerned about the levels of referrals from employers which are investigated but result in no further action by the GMC.
The GMC claimed in its FOI response that it is working to reduce the level of unnecessary referrals:
“We’re supporting the work of our partners to standardise local investigation processes and how these might address disproportionality at the early stages of a concern being raised, to avoid unnecessary GMC referrals.”
However, GMC does NOT collate data about whether referrals that it receives are necessary:
“In respect of your question as to if referrals which ended in advice were necessary, we don’t hold data on whether referrals were necessary…”
This seems half-hearted.
Although the GMC monitors the performance of individual employers through its attached Employment Liaison Advisers, it has not provided any evidence that it systematically uses the information to track differences between organisations and to thus identify outliers.
In response to a question on whether the GMC has plans to track differences between employers’ referral patterns, the GMC strangely referred me to the following document:
GMC Equality, diversity and inclusion Targets, progress and priorities for 2023
The document is about GMC performance targets on tracking how doctors with protected characteristics and related factors are treated, and not differences between employers.
So, whilst superficially adopting the recommendations of the Hooper review, the GMC still protects the powerful through wilful blindness and failure to actively check for signs of abuse. It does not seek to actively identify outliers and seems not to collate nor extract data that would enable comparisons and the identification of outliers. Leaving abusers unpunished is not effective safeguarding of whistleblowers.
And yet GMC received this advice from Hooper in 2015:
“24. The effect of the reprisals on individuals at work and at home is likely to be devastating. Doctors who have devoted their lives to the care of others face the prospect of their careers being brought to an end. One of the consequences may be that the doctor against whom the retaliatory measures are being taken becomes clinically depressed. His or her depression may then be used as justification for further action against the doctor.
25. It is self-evident that the fear of suffering reprisals acts as a powerful disincentive to raising concerns, as does also a belief that the concern will be ignored. The attainment of the objective of patient safety therefore requires that the risk of reprisals is reduced or eliminated, and that concerns are not ignored.”
GMC resisted a suggestion to amend Good Medical Practice for medical managers, to make it a proscribed practice for doctors in leadership positions to carelessly or knowingly make unsubstantiated or false GMC referrals or PPA referrals on doctors whom they manage. GMC claimed that its existing general guidance on conduct is sufficient. Many harmed whistleblowers would likely disagree, based on years of GMC inaction over abusive medical managers.
A telling detail from the GMC’s FOI response is that GMC says it deploys a special protection for referred whistleblowers. It checks whether the referrer’s claims can be corroborated before launching an investigation:
“In the cases where a doctor has raised concerns in the public interest, we seek independent corroboration of the concerns raised by the employer before deciding whether to open an investigation. If a full investigation is needed, we ensure the investigation focuses on independent corroboration of concerns raised by the employer.”
Should the GMC not be doing this for ALL doctors who are referred?
After all, the trauma and serious harmful health effects of a GMC referral and investigation are well known.
In all, the GMC appears to remain establishment-centric. Its bias is towards power. It has implied that it routinely opens investigations without corroboration of employers’ concerns. It appears to have not followed up on many cases where employers’ referrals have not led to a GMC investigation. It avoids data analysis and collation that might reveal rogue employers, and it will not tighten the rules for medical managers to deter vexatious referrals.
None of this should be surprising. The government and NHS England have delayed and watered down the Kark review on Fit and Proper Persons in the NHS, and a recent government release about the East Kent maternity scandal noted that NHS England will only remove erring NHS executives under “extreme” circumstances:
“NHSE has powers regarding the replacement of trust leadership which it uses in extreme and exceptional circumstances, and applies fairly, reasonably and proportionally, and with the interests of those served by the trust in mind.”
I have asked GMC for some further details and clarifications regarding the responses it gave which were vague or evasive.
I have also asked for a list of NHS trusts which since May 2022 have made referrals which did not result in GMC investigation, and the numbers of such referrals made by each of the trusts in question.
RELATED ITEMS
Sorry is the hardest word: CQC, Paula Vasco-Knight and Regulation 5 Fit and Proper Persons
Mr Tristan Reuser’s whistleblowing case: Scandalous employer and regulatory behaviour on FPPR
Waste Industry: The NHS disciplinary process & Dr John Bestley
Can Healthwatch Birmingham please let us see its complaints & concerns data on UHB?
Bewick, the ICB, misinformation by UHB about GMC referrals and a late correction
NHSE, ICB and UHB’s three-ring circus and Rosser’s digital assignment
What the UHB Freedom To Speak Up Guardian told the BBC
Why is CQC not investigating UHB under CQC Regulation 12?


GMC is utterly unfit for purpose and dangerous, perpetuating cover-up and omissions. Claiming to have reviewed cases – without even gaining access to contemporaneous medical records, to establish any facts or events!!
LikeLike
Thanks again for a forensic approach to the failings of managers and the GMC.
I was pleased the ICO overrode the GMC, when trying to withhold data.
We need a voice to hold organisation to account, as you are doing in your articles.
Keep up the good work.
LikeLiked by 1 person