By Dr Minh Alexander NHS whistleblower and former consultant psychiatrist, 20 March 2019
| Summary: In 2017 The government stopped central collection of data on assaults against NHS staff despite a rising trend and much criticism. A year later, it backtracked and announced a violence reduction strategy which included a promise that the CQC would scrutinise NHS trusts’ violence reduction plans. Three datasets show that NHS mental health services staff have suffered the highest rate of assaults. The Health and Safety Executive has supplied FOI data on statutory staff injury reports (RIDDOR) by NHS mental health trusts, which shows that since April 2015, 20 mental health trusts accounted for 67% of all the non-fatal RIDDOR injury reports. According to other FOI data, these 20 trust were mostly higher users of physical restraint, with very marked variation in the rates of resultant injury to staff and patients. However, the physical restraint data they supplied was incomplete and patchy. This raises questions about the governance and regulation of this area. The most recent CQC inspections on these 20 trusts do not report reliably on violence against or injuries sustained by staff. |
BACKGROUND
Amidst condemnation, the government stopped collecting central data on violence against NHS staff in 2017.
This was despite a steady escalation over several years in the number of assaults on NHS staff and questions in parliament about this.
Philip Dunne the then DH Minister of State stated in a written answer to a parliamentary question:
“We continue to collect data on physical assaults against NHS staff through the annual NHS staff survey, with trusts also collecting data at a local level, and we are making crucial legal changes to ensure those who are violent face the full force of the law.”
Some might think this disingenuous because the NHS staff survey does not give a precise idea of the number of assaults against NHS staff, not least because of incomplete response rates. Since 2012 the survey has only asked:
“How many times in the last 12 months have you personally experienced violence at work from patients/ service users, their relatives or members of the public:
- Never
- 1-2
- 3-5
- 6-10
- More than 10”
Included in Dunne’s written answer is this table, which he claimed was evidence of stability in the level of assaults against NHS staff:
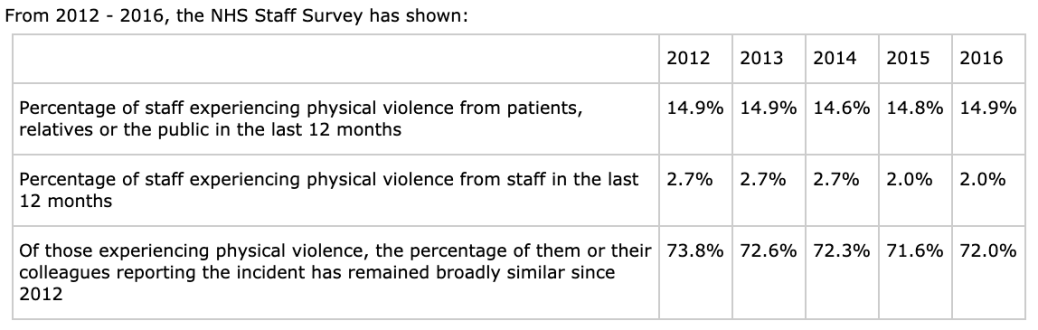
In fact, over the last 10 years the NHS staff survey source data shows an overall increasing trend in the numbers of assaults on NHS staff by the public:

According to NHS staff survey data, NHS ambulance trust and mental health trust staff are most likely to experience violence:
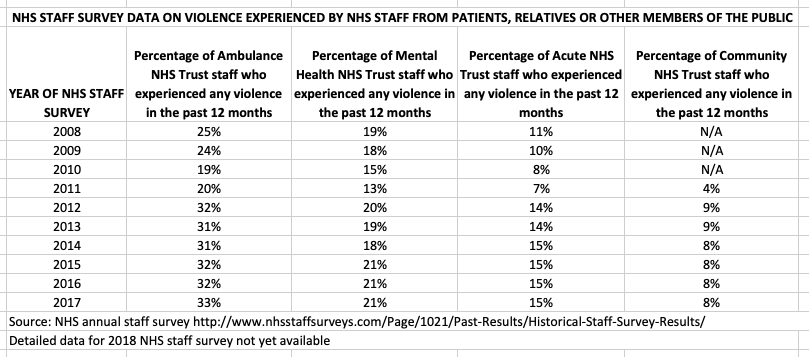
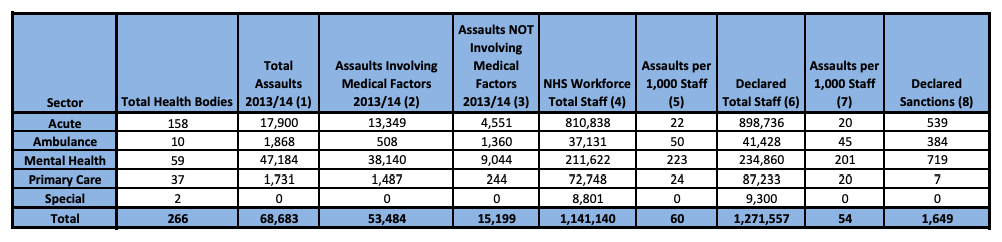
NHS Protect’s pre-2017 national data collection regularly showed that mental health services had the highest rate of assaults per 1,000 staff. These are the figures for 2013/14 which show that mental health trusts had almost 10 times more assaults per 1,000 staff than all other NHS trusts combined (223 assaults per 1,000 staff per year vs 23 assaults per 1,000 staff).
In early 2018, an FOI by the Health Service Journal on behalf of Unison to 181 NHS trusts suggested that the number of reported assaults against NHS staff had increased by 10%, from 51,447 in 2015/16 to 56,435 assaults in 2016/17.
The FOI gave the following figures for assaults in different types of NHS trust in 2016/17, and HSJ compared it against figures from 2015/16 which had been collected by NHS Protect:
| TYPE OF NHS TRUST | 2016/17
(FOI data from 181 NHS trusts) |
2015/16
(NHS Protect data on the same trusts) |
| Acute* (104 trusts) | 18,720 | 15,469 |
| Mental Health* (39 trusts) | 33,820 | 32,746 |
| Ambulance (9 trusts) | 2,330 | 2036 |
| Community (13 trusts) | 860 | 708 |
| Specialist (15 trusts) | 532 | 416 |
| TOTAL | 56,262 | 51,375 |
*Includes combined trusts with community services.
Based on its sample of 181 trusts, HSJ commented that mental health services are:
“…by far the most physically dangerous place in the NHS to work. Staff in mental health trusts are approximately seven and half times more likely to be attacked than staff in other NHS trusts.”
By October 2018 the government managed the controversy about its decision to stop national collection of violence statistics by announcing a strategy to reduce violence against NHS staff. In a speech the Secretary of State promised:
- New legislation: The Assaults on Emergency Workers (Offences) Act 2018 which covers NHS workers as well as other services such as the police and fire services
- Cooperation by the police and CPS to ensure that violence against NHS workers is prosecuted
- Resumed national collection of statistics
- Specific regulation: “CQC will scrutinise NHS trusts’ violence reduction plans”
HSE RIDDOR DATA FOR NHS MENTAL HEALTH TRUSTS
The Health and Safety Executive collates data reported under the Reporting of Injuries, Diseases and Dangerous Occurrences Regulations 2013.
Reporting by ‘responsible persons’ (usually the employer) is mandatory.
Annual HSE RIDDOR statistics suggest that working in health services is moderately risky, and carries a greater risk of reportable non-fatal injury than construction or mining and quarrying:
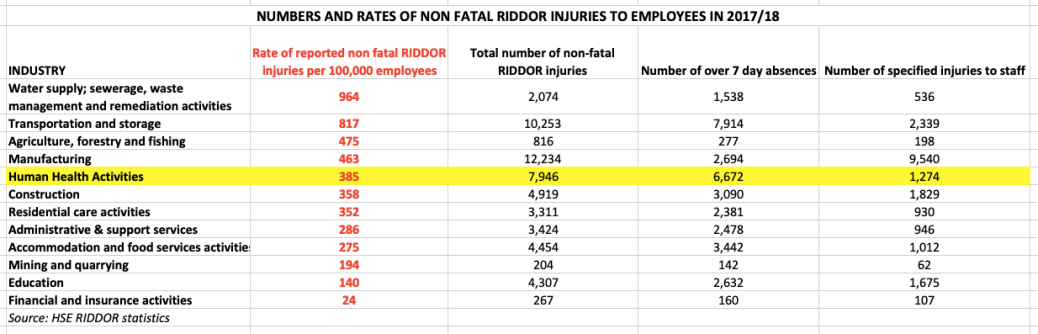
In mental health, injuries to staff can be linked to poor management of patient aggression and violence through failures of risk assessment, prevention and de-escalation, or physical restraint which goes wrong.
Factors such as insufficient staff numbers, over crowding, poor physical environment, lack of therapeutic support services and inappropriate skill mix can contribute to some of these problems.
Where mental health staff suffer injuries related to violence by patients, a concern also logically arises about the care of patients.
I asked HSE for information on recent RIDDOR reports about NHS mental health trusts, including deaths. All deaths due to work-related accident must be reported under RIDDOR, whether the deaths of employees or members of the public.
HSE provided data on:
- Incidents resulting in staff sickness absence over 7 days:
“Accidents must be reported where they result in an employee or self-employed person being away from work, or unable to perform their normal work duties, for more than seven consecutive days as the result of their injury.”
- Incidents resulting in certain significant, specified injuries to staff:
Fractures, other than to fingers, thumbs and toes
Amputation of an arm, hand, finger, thumb, leg, foot or toe
Any injury likely to lead to permanent loss of sight or reduction in sight in one or both eyes
Any crush injury to the head or torso, causing damage to the brain or internal organs
Any burn injury (including scalding)
But no data was provided on deaths. I will pursue this.
The full spreadsheet of raw data disclosed by HSE can be found here.
The data was analysed after removing a few instances of data from acute NHS trusts which had been wrongly included.
Since 1 April 2015, there have been a total of 3,992 ‘over 7 day’ absences and 761 specified injuries sustained by NHS mental health staff that have been reported to HSE.
The summary RIDDOR injury statistics for mental health trusts can be found here.
This is the distribution of non-fatal RIDDOR injuries in NHS mental health services over time:
| YEAR | Number of over 7 day sickness absences | Number of specified injuries |
| 2015/16 | 1,055 | 168 |
| 2016/17 | 989 | 209 |
| 2017/18 | 1,114 | 209 |
| 2018/19 year to date | 834 | 175 |
| Total | 3,992 | 761 |
Unsurprisingly, HSE advises that there is under-reporting of RIDDOR incidents, so the real figures are higher
Over the period 2015/16 to 2017/18, NHS Mental health trusts accounted for 15.4% (3744 of 24212) non-fatal RIDDOR injuries to employees in Human Health Activities.
There was considerable variation between different NHS mental health trusts.
The number of significant, specified injuries in the period varied between 47 at Lancashire Care NHS Foundation Trust, and zero.
Below are the 20 mental health NHS trusts which had the most RIDDOR non-fatal injuries. These trusts accounted for 67% (3182 of 4753) of RIDDOR non-fatal injuries to staff since April 2015.
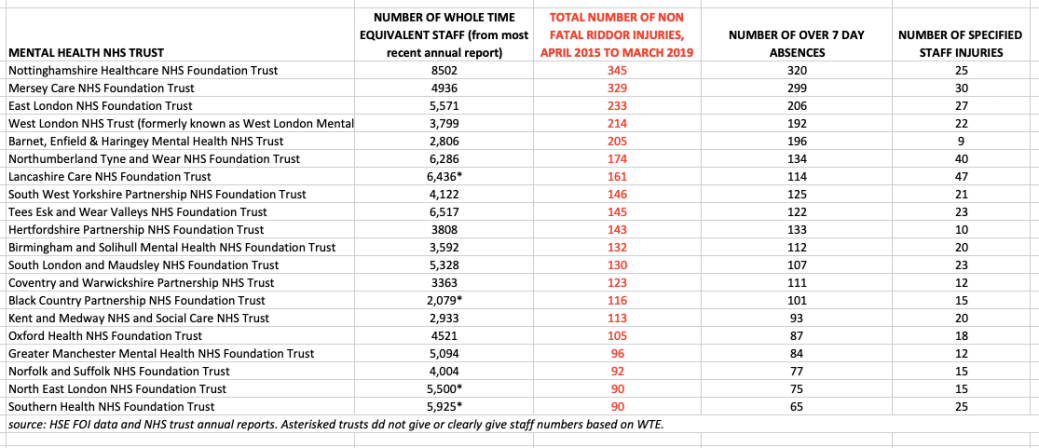
The variation may be explained partly but not wholly by size of trust. ‘Outstanding’ East London NHS Foundation had a total of 233 RIDDOR injuries, but South London and Maudsley NHS Foundation trust which is the same size had 130 RIDDOR injuries.
Mersey Care NHS Foundation Trust is equivalent in size to Leicester Partnership NHS Foundation Trust, but had three times as many absences over 7 days.
Mersey Care NHS Foundation Trust runs Ashworth Hospital, which has high secure 228 beds. Nottinghamshire Healthcare NHS Foundation Trust runs Rampton Hospital, which has 357 high secure beds and West London NHS Trust runs Broadmoor Hospital, which has 240 high secure beds.
However, it is unclear to what extent specialist secure services account for higher numbers of absences over 7 days.
For example, Hertfordshire Partnership is a smaller trust and has 30 medium secure beds but racked up 133 non-fatal RIDDOR injuries compared to 84 at Greater Manchester Mental Health NHS Foundation Trust, which has 118 medium secure beds.
Neither do the RIDDOR injuries seem to be consistently associated with rates of physical restraint.
Examination of FOI data from 2016 on physical restraint of patients in mental health trusts, obtained by Norman Lamb’s office, shows very inconsistent recording of information on use of restraint and restraint-related injuries to staff and patients in the above 20 trusts. Anomalies in the data raise questions about the quality of data provided.
Where data was provided by any of the above 20 trusts, this broadly showed high use of physical restraint compared against the mean (3926 episodes of restraint) for mental health trusts in that period (based on 48 trusts who provided information). The exceptions were Barnet, Enfield and Haringey Mental Health NHS Trust and North East London NHS Foundation Trust, so it is interesting that these trusts were amongst the 20 that generated high numbers of RIDDOR injuries despite reportedly lower levels of physical restraint.
There was marked variation in the proportion of restraint episodes that resulted in recorded injury to staff or patients. If the figures are to be believed, the chances of injury to a member of staff taking part in physical restraint at Nottingham Healthcare NHS Foundation Trust and Mersey Care NHS Foundation Trust was an eye watering 41% and 32.5% respectively.
This purportedly fell to only 2% of restraint episodes resulting in staff injury at Lancashire Care NHS Foundation Trust. But a question arises about this because Lancashire Care racked up the highest number nationally of significant, RIDDOR specified injuries to staff.
Other dubious statistics are Lancashire Care’s claim that zero patient injuries resulted from 7,371 episodes of restraint, and Southern Health NHS Foundation’s claim that only two patient injuries resulted from 10,398 restraint episodes.
The poor and incomplete data on restraint and its consequences and marked apparent variation in rates of resultant injuries suggest that this is a poorly governed and regulated area. But the level of variation does raise questions on whether some of the injuries might be avoidable.
Current CQC inspection reports on the 20 trusts with the most non-fatal RIDDOR injuries do not consistently mention violence against staff and give little hard data about assaults.
The CQC reports also do not refer to staff injuries, (from a search under ‘injury’, ‘injuries’ and ‘RIDDOR’), except in three instances.
At Mersey Care NHS Foundation Trust the CQC observed:
“At core service level, we saw that managers had access to monthly ‘dashboards’ that illustrated their team’s performance in a number of areas. These areas (or key performance indicators) included mandatory training, patient experience scores, staff sickness, staff injuries, patient harm and other incidents.”
At Coventry and Warwickshire Partnership NHS Trust the CQC observed:
“The trust had not addressed the issue of access in to the seclusion room through an area which was too narrow for staff and patients to enter without the potential for injury.”
“The trust must ensure that changes are made to the seclusion room to prevent the risk of injury to patients and staff.”
At North East London NHS Foundation Trust the CQC observed:
“However, the majority of incidents involving patients physically attacking staff were recorded as ‘no harm’ despite many staff receiving injuries.”
At South London and Maudsley NHS Foundation Trust the CQC commented on injuries to patients due to restraint, but not staff injuries:
“The trust should ensure staff record incidents of restraint accurately including the type of restraint, position of restraint, members of staff involved, length of time the restraint took place and whether the patient received a physical health check for any injuries post restraint.”
In an inspection report of 1 March 2019 on Kent and Medway NHS and Social Care Partnership Trust, published after the Secretary of State promised that CQC would target violence against NHS staff, CQC made no mention of such matters.
It would seem that CQC is either not consistently examining and or reporting on violence and injuries to staff in NHS mental health services.
So much for the government’s promise that CQC would help enforce violence reduction. But it is not surprising because the government has form for waving the CQC about tokenistically, to defuse political pressure.
This data will be submitted to parliament and I will draw CQC’s attention to the RIDDOR data for mental health trusts.
CORRESPONDENCE TO PARLIAMENT & CQC 21 MARCH 2019
Joint Committee on Human Rights
From: Minh Alexander <REDACTED>
Subject: HSE RIDDOR staff injury data for NHS mental health trusts 2015/16- 2018/19 YTD
Date: 21 March 2019 at 08:24:58 GMT
To: Edward Baker <REDACTED>
Dear Ted,
HSE RIDDOR staff injury data for NHS mental health trusts 2015/16- 2018/19 YTD
I forward this FOI raw data from HSE on RIDDOR injuries to the staff of NHS mental health trusts for CQC’s information, in the event that CQC does not track this data:
I assume that CQC does not track it, as HSE itself does not track it.
This is the analysed data, cleaned of some data on NHS acute trusts which was wrongly included, and broken down by individual mental health trusts:
You will see that there is great variation.
With best wishes,
Minh
Dr Minh Alexander
RELATED ITEMS
Letter to parliament: CQC’s inconsistent regulation of restraint in mental health
Safe in their hands? Government’s response to coroners’ warnings about the NHS
4 years of CQC mental health whistleblowing data
St. Andrews Healthcare, Whistleblowing, Safeguarding and Public Protection


I realise that this must be an exceptionally important post but have insufficient time at the moment to do anything but glance through it.
I shall hope to read it properly later in the week. In the meantime, I thank you for finding, gathering, recording and publishing these concerning facts.
LikeLike
Hancocks 1/2 hr is not so funny now!
LikeLike