By Dr Minh Alexander NHS whistleblower and former consultant psychiatrist, 16 February 2018
On 23 February 2018 a preliminary hearing will take place of a whistleblowing Employment Tribunal claim against St. Andrews Healthcare. The hearing will take place in private at 10 am Cambridge County Court, for two hours. The claim is by Noel Finn, who who previously whistleblew about Yarl’s Wood Immigration Removal Centre. He tweets at @Nolliag66
Some background data on whistleblowing, Safeguarding and public protection issues in relation to St Andrews Healthcare is presented below.
Policy background
The NHS has shut down all its asylums and has lost many of its mental health beds:

Graph of NHS Mental Health beds via Professor Brian Jarman
Every day there are hundreds of acutely unwell NHS mental health patients in out of area placements, hundreds of miles from home. This is inherently risky as it removes patients from normal support networks, and affects clinical communication and planning. In 2016 the National Confidential Inquiry into Suicide and Homicide described the risk associated with discharge from out of area placements and advised that acutely ill patients should not be sent out of area:
“90. 195 (9%) died after being discharged from a non-local in-patient unit. This proportion increased to 11% (67 cases) of those who died within 2 weeks of discharge. The number of suicides after discharge from a non-local unit increased from 85 (8%) in 2004-2008 to 96 (10%) in 2009-2013.”
“Key elements of safer care in mental health services…No ‘out of area’ admissions for acutely ill patients”
The mental health deinstitutionalisation movement was well-meant and predicated on government promises to fund good quality care in the community, but these never fully materialised. As one leading light of the NHS de-institutionalisation programme once said ruefully:
“Any fool can close an asylum”.
In fact, a programme of mental health investment to deliver a National Service Framework of quality standards, introduced in 1999, has been reversed under the current government. Essential services for helping people with serious illness to cope, such as assertive outreach teams and day hospitals, have been shut down or diluted.
The most seriously ill patients with the most complex needs have sometimes ended up in prison or secure psychiatric care as a result of not receiving adequately proactive care in the community.
St Andrews Healthcare is a large private mental healthcare provider that mainly provides specialised inpatient care for patients detained under the Mental Health Act, but also provides some acute general care. It mops up need that is not accommodated by the NHS and its patients are almost wholly NHS funded:
“The Charity receives essentially all its income from NHS entities.”
St Andrews Healthcare Annual Report 2016/17
St Andrews reports that NHS England is its biggest funder. NHS England’s spending transparency data shows that it has directly purchased at least £294,796,282.22 of services from St Andrews Healthcare over the period January 2014 to July 2017. (For some reason, NHS England’s spending transparency data on purchases over £25K stops after July 2017). £300m is almost the annual budget for three NHS mental health trusts.
NHS England direct spending on St. Andrews Healthcare services (purchases over £25K):
| Year | Amount spent directly by NHS England on services by St. Andrews Healthcare |
| 2014 | £ 45,354,111.47 |
| 2015 | £ 89,938,611.82 |
| 2016 | £ 103,238,855.07 |
| 2017 to July | £ 56,264,703.86 |
| Total | £294,796,282.22 |
Source: NHS England spending transparency data
Extracted data for St. Andrews Healthcare: NHS England spend over £25K on St Andrews Healthcare January 2014 to July 2017
The main site, St Andrews Hospital in Northampton, was the old county asylum and traces of its history remain in that it has a Court of Governors. According to the CQC, the main St Andrews hospital site in Northampton currently has 659 beds.
The hospital is a powerful institution and a significant part of the local economy in Northamptonshire.
St Andrews has swum against the tide of de-institutionalisation. Some may object to institutional care per se, and perceive all detention as oppressive. Indeed, poorly prescribed and delivered care in detained conditions can be harmful, cause disability and may increase disturbed behaviour. But there is nothing innately wrong with institutional care, if it is of high quality and delivered strictly according to need. Some people have highly complex needs and need the sanctuary of a locked environment to manage all the risks associated with their clinical conditions. Moreover, the Mental Health Act can safeguard rights to care and importantly, to aftercare in the community once detention ends.
Providing care in closed environments is challenging. Staff need to be well trained and well led to cope with the nature of the work, to ensure that care is therapeutic, and not custodial or punitive. Institutions can very easily take on a life of their own, and develop an unhealthy culture that subverts their original mission. Repeated inquiries into prison and mental health failures attest to that. For example:
Ashworth Special Hospital: Report of the Committee of Inquiry
Added to this is a context of low societal expectations and disparity of esteem, which can affect staff as well as patients. As the 2009 Healthcare Commission into West London Mental Health Trust noted:
“many services were starting from a low baseline and, despite these initiatives, the need for modern mental health services remains a relatively low priority in society”
St Andrews Healthcare had a good reputation nationally for many years for highly specialised care of very challenging behaviour and complex need. Latterly, its business model changed and it expanded greatly. It was incorporated in 2004 and published annual accounts show that income has increased from £80,936,000 in 2004/5 to £205,600,000 in 2016/17. There have been some concerns over quality and governance since this expansion.
Concerns about St. Andrews
In 2011 there were a cluster of four deaths within a six month period on Grafton ward, a long stay, locked male ward at St Andrews Northampton. These deaths remain an unresolved concern because NHS England refused to ensure that the deaths were investigated as a cluster, despite intervention by Healthwatch England.
Letter by NHS England to Healtwatch England 14 August 2014
Letter by Healthwatch England to NHS England 8 December 2014
NHS England letter to Healthwatch England 8 January 2015
Letter by Anna Bradley Chair of Healthwatch England to Simon Stevens CEO NHS England 2 February 2015
“Fifteen months after NHS England committed to carrying out the review into St Andrews, nothing has emerged and I am frankly concerned at the lack of action and urgency shown by NHS England on ensuring that lessons have been learnt and appropriate action taken”
Anna Bradley to Simon Stevens 2 February 2015
There is limited information in the public domain about these deaths, but concerns have been raised by several parties about the rigour of investigations to date, including by whistleblowers.
Sara Ryan mother of Connor Sparrowhawk who died in the care of Southern Health NHS Foundation Trust received a copy of the internal St Andrews report.
Four deaths heads and a medical director
Of concern, the CQC rated the Mens Service at St. Andrews where the four deaths occurred was rated as fully compliant at the time of the deaths, and also shortly afterwards in 2012:

But by August 2017, the CQC rated the St. Andrews Mens Service at Northampton as ‘Inadequate’ , commenting that the provider had not responded adequately to previous CQC concerns.
Bill Johnson, one of the four Grafton ward patients who perished, died through severe constipation. Mr Mark McGhee, the lawyer for Bill Johnson’s family, was reportedly critical of both his care and the system response to his death, including the CQC’s failure to investigate:
The systemic issues underlying such deaths of vulnerable adults have been raised once more by the inquest on Richard Handley’s death on 8 February 2018.
In 2013, St. Andrews was warned about safe staffing on its child and adolescent wards, support for staff and other matters:
In 2013, HSCIC data from a government census of Learning Disability services showed that of 241 patients receiving care from St Andrews Healthcare, 70 (29%) had been secluded, 95 (39%) had been restrained and 30 (12%) had been physically assaulted in the three months up to September 2013.
In January 2014, it was reported that a St. Andrews nurse who grabbed a patient’s throat, and would not let go, was struck off.
In 2015, St. Andrews was warned about its use of prone (face down) restraint. This is because it is government policy that this should be used minimally and for the shortest time possible , because prone restraint is dangerous to patients.
In February 2017 concerns were raised by the Channel 4 Dispatches programme ‘Under lock and key’ , which asked whether the care at St. Andrews for young people with learning disabilities and autistic spectrum disorders was excessively restrictive and might actually be causing behavioural problems. Importantly, a high use of prone (face down) restraint was revealed: 600 instances of prone restraint on young people over a six month period.
In March 2017 the Bureau of Investigative Journalism reported that St. Andrews was charging some families top up fees, in addition to substantial fees already paid by the NHS, for extra care beyond that which the home area authorities were prepared to fund. One mother, who lived hundreds of miles away, was reportedly charged £64 a day in return for extra care to encourage her daughter to increase physical activity.
|
Another mother told the Bureau of Investigative Journalism: “A mother whose son is currently a patient at St Andrew’s, who asked to remain anonymous, said she had repeatedly complained about her son’s weight gain. She claimed that denying access to exercise facilities was used by staff as a form of punishment for infringement of strict behavioural rules. “My son became clinically obese in less than a year at St Andrew’s,” she claimed. St Andrew’s website claims that patients get more than “the recommended 25 hours of meaningful activity” and a spokesman told the Bureau patients were encouraged to exercise. “I questioned them about this ‘25 hours’ thing and was told that eating – breakfast, coffee break, lunch, snack time, dinner – are counted as meaningful activities,” the mother said. She said patients had to be escorted to use the gym and other facilities, use of these facilities was seen as a privilege, and staff shortages meant there were often insufficient personnel to act as escorts, she claimed. “My son’s need for exercise should have been seen as a medical emergency and not a privilege he needed to work towards,” she said. After repeatedly complaining, she said her son’s treatment improved. “But I fear for patients without people on the outside who can make a fuss on their behalf,” she said.”
|
In November 2017 it was reported that the coroner criticised St. Andrews and others over the death of Stephen Martin, who was died three days after being discharged from St. Andrews on a Community Treatment Order.
Whistleblowing by St. Andrews staff to the CQC
The CQC disclosed national data on whistleblowing contacts from all registered providers for the period 2015/16 and 2016/17.
Extracting the data for St Andrews Healthcare gives 19 whistleblowing contacts over this two year period, 15 of which related to the Northampton site.
Whistleblowing contacts to CQC by St. Andrews Healthcare staff in 2015/16 and 2016/17:

Safeguarding at St. Andrews
I asked for data from Healthwatch Northamptonshire, Northamptonshire County Council and Essex County Council.
Information from Healthwatch Northamptonshire
Healthwatch Northamptonshire gave information as follows:
“2014/15 – no negative feedback received about St Andrew’s Healthcare
2015/16 – 7 issues raised with us by patients or relatives
2016/17 – no negative feedback received about St Andrew’s Healthcare
2017/18 year to date – no negative feedback received about St Andrew’s Healthcare
The seven issues raised in 2015/16 can be summarised as follows: one safeguarding (this is a correction to my previous response, we have made one safeguarding referral), three patients unhappy with aspects of care or treatment, one concerned relative and one member of the public re. social media comments.”
Information from Northamptonshire County Council
This the disclosure correspondence from the council: FOI response FR7861 by Northamptonshire County Council
Child Safeguarding referrals:
The Council declined to provide data for the five years 2010/11 to 2014/15 on the basis that it did not hold digital records for these years and a search would have exceeded the cost limits.
For the years since 1 April 2015, the council has received the following number of Child Safeguarding concerns relating to St. Andrews:
| Year | Number of Safeguarding concerns received about care at St Andrews Healthcare | Number of concerns upheld or partially upheld |
| 2015/16 | 45 | 7 |
| 2016/17 | 26 | 8 |
| 2017/18 | 26 | 8 |
| Total | 97 | 23 |
In regards to the Council’s response to Channel 4’s ‘Under Lock and Key’ investigation, this is the action that it reportedly took in response:
“The Northamptonshire Safeguarding Children Board (NSCB) discussed the BBC Panorama programme on St Andrews Healthcare, based in Northampton, at Board meetings and took the following actions:
- Reassurance from the regulatory bodies (Ofsted, Care Quality Commission and NHS England) that they had taken consideration of the programme in their inspection and monitoring visits. This reassurance was provided both in writing and verbally. The Independent Chair of the Board personally spoke to senior representatives of the organisations.
2. Considered the subsequent Ofsted inspection of the adolescent facility at St Andrews, which contained no concerns regarding immediate safeguarding issues at the unit.
- Responded to a letter from a member of the public which referenced concerns about safeguarding practices at the adolescent unit. These concerns were based on a visit to the unit prior to it formally opening. These concerns were relayed to the senior management representative at St Andrews, who is a full member of the NSCB. A satisfactory response to these concerns was received and the Board was assured that the potential safeguarding problems outlined in the letter had been addressed.
- The Independent Chair of the NSCB visited St Andrews and discussed these concerns with the Head of Safeguarding, seeking and obtaining further assurance.
- Members of the NSCB have been invited to visit the unit and to meet with both managers and staff.”
Reassurance from the CQC? This is what Bill Kirkup said about ‘circular’ assurance in the Morecambe Bay maternity scandal:
The Report of the Morecambe Bay Investigation
“5.162 Assurance had become circular. The CQC was taking reassurance from the fact that the PHSO was not investigating; the PHSO was taking assurance that the CQC would investigate, the NW SHA was continuing to give assurances based in part on the CQC position. Monitor asked for assurance and received the perceived wisdom – that the issues were under control and minimal. At no time did Monitor question these circular arguments or the improbability of cultural concerns being resolved within six months.”
Adult Safeguarding referrals:
Abysmally, the Council claimed that its systems could not support an easy search:
“Data around providers is not currently something that we are able to pull easily from the system due to the fact that provider detail is not available on the client’s assessment within the ‘source of risk’ section in a reportable format.
Information could be entered on the assessment as any number of things within the ‘Name/Organisation’ question of the assessment i.e. name of person, team, organisation, ward etc. all of which could be St Andrews but not listed as St Andrews. We would therefore need to undertake a manual search of all relevant records in order to locate any information matching the criteria and parameters of question 4.”
Accordingly, the Council refused to disclose any Adult Safeguarding data on the basis that it would exceed cost limits.
We are to believe that Northamptonshire CC has a huge hospital site with over 600 highly vulnerable, locked up people on its doorstep, and it cannot tell easily whether the custodian may have been mistreating any of these vulnerable adults.
I must question the Council’s claim that it was unable to search easily for Adult Safeguarding data in relation to St. Andrews. Its 2016/17 Adult Safeguarding Board report shows that it holds aggregate data on Safeguarding contacts relating to St. Andrews. For quarters 1,2,3 and 4, Adult Safeguarding contacts from St. Andrews accounted for approximately 6.5%, 7%, 4% and 6% of a total of all sources of concern.

Bar chart from Northamptonshire Adult Safeguarding Board annual report 2016/17
In 2016/17, Northamptonshire CC received a total of 6,392 Adult Safeguarding concerns. Extrapolating roughly from the above bar chart and assuming St. Andrews was the source for approximately 5% of these concerns, this gives a rough figure of 319 Adult Safeguarding concerns relating to St Andrews. And yet the Council says it is not tracking this activity.
I am writing to the Council to query its claims that it cannot produce the requested data on Adult Safeguarding concerns about St. Andrews.
Of additional concern, the Council disclosed that there had not been any serious case reviews on adult cases in the last 10 years:
“There have not been any Serious Case Reviews in the last 10 years involving St Andrews Healthcare.”
This is surprising given the cluster of four deaths on Grafton ward.
According to the Council,
“A Safeguarding Adults Review (SAR) was concluded in September 2016 and published June 2017 where the individual concerned had spent some time at St Andrews.”
This is the only published SAR on the Northamptonshire Adult Safeguarding Board webpages that may correspond to the above report, but I am awaiting confirmation from the Council that this is indeed the report:
Northamptonshire Adults Safeguarding Board, Safeguarding Adults Review on ‘Claire’
The report favourably mentions a period of care at St. Andrews from 1994 to 2010 in which a patient made progress.
Information from Essex County Council
St Andrew’s Healthcare site in Essex reportedly has 79 beds.
Essex County Council advised that a total of 67 Safeguarding concerns had been received about the St Andrews service since 2011, 25 of which had been had been upheld or partly upheld.
| YEAR | Number of Safeguarding concerns received |
| 2011/12 | 1 |
| 2012/13 | 10 |
| 2014/15 | 13 |
| 2015/16 | 31 |
| 2016/17 | 12 |
| 2017/18 | 0 |
| Total | 67 |
A patient, Beverly Higgins, died on escorted leave from St Andrews in 2008, but Essex County Council claimed that it held no Safeguarding data about this. The police reportedly investigated in 2009 with respect to potential corporate failures of duty of care.
A St Andrew’s Healthcare spokesman was quoted by the Basildon, Canvey and Southend Echo about the death:
“St Andrew’s Healthcare, an established charity specialising in mental health care and rehabilitation, is co-operating fully with police and external enquiries into this tragic incident.
“It takes confidence, in the light of an independently commissioned investigation, that there will be no finding of culpability on its part and is satisfied with systems and structures in place to safeguard the well-being of those in its care.”
Essex County Council advised that there had been no Serious Case Reviews on deaths of St. Andrews patients.
Public Protection
The other side of the Safeguarding coin is public protection. This is particularly relevant to the Northampton site where the hospital, which houses many mentally disordered offenders, some subject to Section 41 Home Office Restriction Orders, is situated in the town centre near residential areas. Risk management and patient absconding are of special local sensitivity.
Risk management in such cases is a skilled and challenging task. Therapeutic risk-taking, must be carefully balanced with public protection.
These are some of the past escapes by St. Andrews patients that have come to press attention:
‘Paedophile on unescorted leave from secure unit tried to rape boy’
‘Warning over men on the run from hospital’
‘Another mental health patient goes on run from hospital’
‘Two patients abscond from St Andrew’s mental health unit at Rainworth’
‘St Andrew’s Hospital patient caught after running out of breath following attack on staff’
‘Residents demand improved security at mental hospital’
‘Paedophile’s freedom bid opposed by cops’
Absconding by patients is not of itself evidence of poor care and risk management, as all care needs to contain an element of therapeutic risk-taking in order to be fair and therapeutically effective. However, it is important that private providers like St. Andrews, which draw from the public purse, can transparently demonstrate sound governance, monitoring and learning from any adverse events.
I asked both Northamptonshire and Essex police for information on calls to incidents at St. Andrews but at the time of writing, I have received no data.
A past analysis of absconding from the Northampton site over a three year period gives a rough idea of frequency, albeit these figures relate to a much smaller number of beds than now exist at the site:

Absconding of patients from an independent UK psychiatric hospital: A 3-year retrospective analysis of events and characteristics of absconders, Dickens and Campbell, Journal of Psychiatric and Mental Health Nursing 8(6):543-50 · January 2002
I have not found any published, recent audit or analysis of absconding by patients from St. Andrews facilities.
Due diligence by the NHS
NHS England tethered itself more firmly to St Andrews with a joint venture, as announced via an item on the Birmingham and Solihull Mental Health NHS Foundation Trust website on 19 July 2016:
West Midlands successful in bid to provide innovative secure mental health service
“A partnership of mental health care providers in the West Midlands has been announced by NHS England as one of just four in the country to be successful in a bid to develop a new and innovative model of care for adults in secure mental health services.
The three core partners – Birmingham and Solihull Mental Health NHS Foundation Trust, South Staffordshire and Shropshire Healthcare NHS Foundation Trust and St Andrew’s Healthcare – currently provide all adult secure inpatient services in the region. They have come together formally for the first time to develop a transformational new model, ‘Reach Out’, which will be supported by a range of NHS, charitable and private sector providers.
There are approximately 600 people from the West Midlands currently in medium or low secure care, of whom around 40 per cent are cared for in units outside of the region. The new model will introduce a more personalised intensive outreach service and provide comprehensive and responsive support in the community. This will focus on aiding recovery, enabling earlier discharge and reducing the likelihood of readmission to hospital. As well as clinical care, the new service will provide practical support such as accommodation, community activities, social networks and employment advice. As a result, outcomes for service users will improve and inpatient beds will be freed up to allow those currently placed out of the area to be brought back to the West Midlands, closer to their home and family. It is estimated that, in the first two years alone, around 90 people from the West Midlands will come back to the region for their inpatient care.”
There was a corresponding NHS England press release on the same date.
What due diligence does the NHS undertake when contracting from private sector providers like St. Andrews? I have found no published details other than references in St. Andrews annual reports to CQUIN targets:
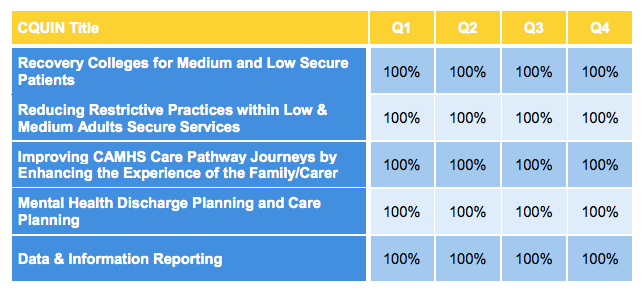
From St. Andrews Quality Account 2016/17
However, as a former St. Andrews whistleblower (see declaration of interest) I found that NHS commissioners and teams from home areas rarely took much interest once patients were placed. Few regularly made the long trek to care plan review meetings. It seemed to me that broadly speaking, the NHS took an out of sight, out of mind approach. This is understandable at one level when the NHS is so hard pressed, but it is not a recipe for Safeguarding success. The geographical separation can certainly be very distressing for families who feel more powerless when they have concerns to raise.
What the government should do of course is re-stock NHS beds and in house expertise in the competent care of the most serious mental illness. But I doubt I shall see that in my life time. Why bother when there are prisons and convenient corporate alternatives.
I suspect there would need to be an extreme nadir before the pendulum swings back.
Assuming there will still be an NHS.
Declaration of interest: I am a former St. Andrews whistleblower. I was employed as a Consultant Psychiatrist in Rehabilitation Psychiatry at St. Andrews between 2003 and 2007 in the Mens service, looking after patients on a slow stream low secure rehabilitation ward and a medium secure admission ward. I occasionally covered for colleagues’ annual leave, which at times included Grafton ward. During my employment, I raised issues of quality of care and Safeguarding.
RELATED ITEMS
4 years of CQC mental health whistleblowing data
UK Whistleblowing Law is an Ass: Helen Rochester v Ingham House Ltd and the Complicit CQC


Thank you for this incredible information, all accessible in one place, shame you do not have a reblog button, but will link in to my blog posts on St Andrews.
Sadly, this appears successive governments policy ie right and left wing, to create these huge institutions, be they charitable or corporate, that are unaccountable, making billions and too big to fail..
I feel St Andrews may just now be taken over by corporate and all will then be hidden with little change for service user or cost to public purse.
Thank you Best Wishes Finola Moss
LikeLiked by 1 person
Agree Dr Aloexander has surpassed herself! Thank you Dr A
LikeLike
I found this post too heart-breaking to study at the length it deserves.
Non-accountability yet again and those who regulate unable so to do.
Shame on everyone involved.
I thank you for your courage in researching and posting.
I can do nothing other than weep.
Kindest, Zara.
LikeLiked by 1 person
My 29 yr old son died at WLMHT where a Healthcare Commission ( just before CQC) investigation into general Patient Safety showed inpatients were “sleeping on couches as no beds were available” and the Director of Nursing said at time “at least we are keeping them off the stre4ts”……….the culture is so wrong!
LikeLiked by 1 person
So very sorry for your loss.
And so very sorry that you have to witness the inadequacy of the response.
The ‘culture’ is indeed wrong – very little evidence of ‘culture’ at all.
As for the Director of Nursing – may well be keeping ‘them’ off the streets, and indeed, keeping Directors of Nursing on a jolly good salary.
Shame on them.
My kindest wishes to you.
LikeLike
I can’t imagine what it feels like Dee, after all these years, seeing the same things happening. It is a major challenge to explain to the public why sound mental healthcare is worth funding, but it is an issue that affects most families at some point.
LikeLiked by 1 person