By Dr Minh Alexander, NHS whistleblower and former consultant psychiatrist 2 October 2016
NHS managers “look up, not out”, so said a major report that was suppressed by the Department of Health. [1] On that theme, the Care Quality Commission has a political function: to flatter politicians and help manage potential embarrassment. It has made arbitrary and inconsistent decisions, which has brought it into conflict with providers, complainants and whistleblowers. CQC has said all the right things about the importance of good complaints handling and transparency, but a review of CQC’s annual reports shows that the CQC has provided little information about why people complain about CQC and what CQC has learnt from the complaints.The data that CQC has released about complaints is not presented in a consistent format and mostly lacks detail. There is limited evidence to demonstrate that CQC has made changes in response to complaints and that it does not repeat mistakes.
The health watchdog the Care Quality Commission was created to replace its more effective predecessors, who had embarrassed the government. Notably, CQC’s immediate predecessor the Healthcare Commission (HCC) had uncovered the grave care failings Mid Staffs, and strategic failures which had contributed to the scandal. The excellent HCC investigation report by Dr Heather Wood et al can be found here: hcc-investigation_into_mid_staffordshire_nhs_foundation_trust
CQC disbanded the central investigation team it inherited from the HCC, which had been so effective. [2] Notoriously, CQC also gagged Dr Heather Wood [3] – this became the subject of much criticism in the public inquiry into Mid Staffs. One interpretation of these events is that the CQC did not wish to be fully “sighted” on politically embarrassing provider failures.
CQC under-uses and frequently minimises its investigatory powers. It has sometimes made misleading claims that it cannot investigate at all. However, it has powers to investigate under Section 48 of the Health and Social Care Act 2008 [4] and it has powers to investigate in relation to patients subject to the Mental Health Act. Whistleblowers and complainants often feel fobbed off when the CQC refuses to do anything at all, except to note their concerns.
There have also been controversies where providers have felt unfairly treated by the CQC, in terms of oppressive inspection approach, increases in CQC’s fees, unfair ratings and excessive factual inaccuracies in CQC reports. [5] [6] Most recently, there was an outcry and many questions when Dr David Zigmond’s practice was shut down. [7] This happened after Dr Zigmond published a book the previous year entitled “If you want good personal healthcare – see a vet”. He wondered whether this “had been a black mark against him”. In 2014, before the publication of Dr Zigmond’s critique of the direction of health services, the CQC had rated his practice fully compliant and noted very positive feedback from patients: “People we spoke with were very happy with the treatment they received at the surgery”.
So how does CQC perform when people complain about it? CQC previously stated that it intended to model best practice on complaints handling:
“We intend to become a role model in the way we ourselves handle and resolve complaints about CQC and concerns raised by our own people.” [8]
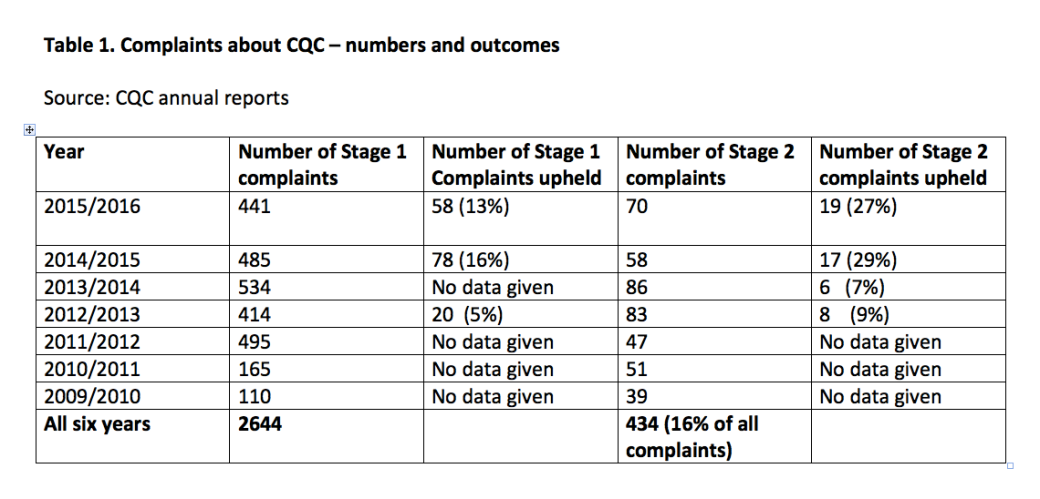
However, a look at the six annual reports published so far by the CQC since its inception raises questions about whether CQC is a good role model. Data in these reports is presented with CQC’s trademark inconsistency, which obscures as much as it reveals. [9] [10] According to the six annual reports, 2644 complaints have been made about CQC between 1 April 2009 to 31 March 2016, and 434 (16%) of these complaints proceeded to Stage 2 of CQC’s procedure. Half of CQC’s annual reports were totally silent on the numbers of complaints upheld at Stage 1 and Stage 2. See table 1 below.
Almost no evidence was provided about the experience of complainants or how satisfied they were with CQC’s complaint handling. This seems a significant omission as CQC has placed an emphasis on the experience of people who complain about regulated bodies:
“ From now on, we will ask providers to share with us any survey they have carried out of people who have complained to them in the last 12 months.”[11]
Has CQC failed to practice what it preaches by not carrying surveys of its own? Or has it surveyed its own complainants, but failed to transparently share the results?
In some years CQC gave a rough indication of the nature of complaints, but in two of the years, no information was provided at all. The most detailed report about complaints was provided by the CQC annual report of 2012/2013, but this was an exception. See Table 2 below.
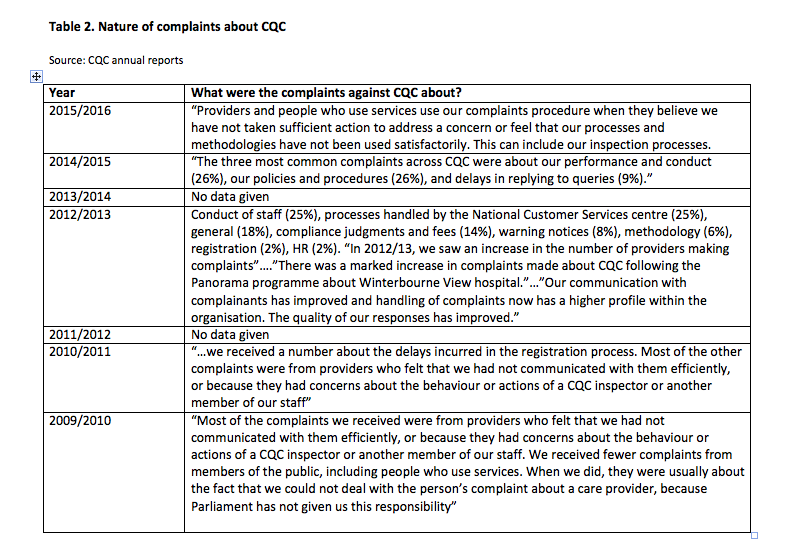
No systematic reports have been provided by CQC on how it has learnt from complaints, made changes or stopped making the same mistakes. Perhaps the most interesting data, analysis of the nature of complaints that were upheld and CQC’s responses to these upheld complaints, is not provided apart from a few selected anecdotes.
CQC’s thematic review report “Complaints Matter” [9] noted that in October 2014, CQC introduced a mandatory ‘key line of enquiry’ in its inspections on how well providers are handling complaints.
CQC also stated in this review report: “We now have a clear vision of ‘what good looks like [on complaints handling]”. CQC added that evidence of good complaints handling would result in complainants being ready to complain again if needed, that complainants would feel fairly treated, that complainants would encourage others to complain if needed and that complainants can see how their complaints have helped to improve services.
So where is the equivalent evidence on CQC’s own complaints handling? Is it too awkward to publish because it might show that the CQC – and its masters – have little intention of changing how CQC does business?
CQC said in 2014 that it would rate providers’ complaints governance as follows:
- Outstanding – there is active review of complaints and how they are managed and responded to, and improvements are made as a result across the services.
- Good – it is easy for people to complain or raise a concern and they are treated compassionately when they do so.
- Requires improvement – people do not find it easy to complain or raise concerns, or are worried about raising concerns or complaining. When they do, a slow or unsatisfactory response is received.
- Inadequate – there is a defensive attitude to complaints and a lack of transparency in how they are handled. People’s concerns and complaints do not lead to improvements in the quality of care.
So, where would you place the CQC on this scale?
Items to cross-reference
PHSO has the CQC’s back
Between April 2009 and September 2015, the PHSO received 354 complaints about CQC, not one of which had yet been upheld as of September 2015. See here for more:
Letter to Health Committee 3 October 2016 about CQC’s handling of complaints
letter-to-house-of-commons-health-committee-3
References
[1] Achieving the vision of excellence in quality, Recommendations for the English NHS system of quality improvement, Institute of Health Improvement, January 2008
ihi-report-achieving-the-vision-of-excellence-in-quality-2
[2] Stafford hospital investigator berates CQC regulator, John Carvel, Guardian, 1 May 2012 https://www.theguardian.com/society/2012/may/01/stafford-hospital-investigator-berates-cqc-regulator
[3] Health watchdog put 20 gagging orders on staff, Patrick Sawer and Laura Donnelly, Telegraph 30 June 2013 http://www.telegraph.co.uk/news/health/heal-our-hospitals/10150664/Health-watchdog-put-20-gagging-orders-on-staff.html
[4] CQC FOI disclosure of 15 January 2016 about six Section 48 investigations conducted since inception https://minhalexander.com/2016/09/27/cqc-foi-disclosure-15-january-2016-about-section-48-investigations-conducted-since-inception-in-2009/
[5] Public Accounts Committee inquiries on CQC 2012 and 2015
[6] Practices to pay almost £2,000 more in CQC fees from April, Jaimie Kaffash, Pulse 30 March 2017 http://www.pulsetoday.co.uk/your-practice/regulation/cqc/practices-to-pay-almost-2000-more-in-cqc-fees-from-april/20031484.fullarticle
[7] The ousted doctor: “My patients’ souls matter the most”, Angela Neustatter, Guardian 18 September 2016 https://www.theguardian.com/society/2016/sep/18/the-ousted-doctor-my-patients-souls-matter-most
[8] CQC annual report 2013/2014 https://www.cqc.org.uk/sites/default/files/20140708-cqc-annual-report-web-final.pdf
[9] How safe are NHS patients in private hospitals? Prof Colin Leys and Prof Brian Toft, Centre for Health and the Public Interest, November 2015 https://chpi.org.uk/wp-content/uploads/2015/12/CHPI-PatientSafety-Dec15.pdf
[10] CQC deaths review: All fur coat. Minh Alexander 13 August 2016 https://minhalexander.com/2016/09/25/cqc-deaths-review-all-fur-coat/
[11] Complaints Matter. CQC thematic review December 2014 http://www.cqc.org.uk/sites/default/files/20141208_complaints_matter_report.pdf


CQC told me that they had investigated my complaint (about the appalling conditions my grandmother was found to be in on multiple occasions at her former care home) When I pressed for details of this “investigation”, it was admitted that they had not visited the care home and that instead they’d relied on a report from the safeguarding team of the local authority – who had taken almost 2 weeks to respond to the alert, and then notified the care home of their visit – no surprises that conditions at the care home were considered acceptable.
We’ve since seen FOI material where the safeguarding team concluded that the reason we’d complained is because we were annoyed that my grandmother had been given notice to leave! They learned this from the social worker.
In fact we spent the next few months insisting that she moved to another care home, against huge opposition from social services and the care home – even though the manager issued a notice to leave whenever we perisisted (civilly) with our questions.
Thank God (!) she broke her hip – once she was in hospital, she began to eat and regain weight and her mental and emotional state improved hugely.
We then had confirmation that she wasn’t dying of cancer – the manager of the care home had told us this lie several months previously.
I can only assume this was to distract us from continuing to ask for answers to our questions, and to explain the drastic weight loss.
She is now happily settled at another care home, has regained weight and is noticeably happier…however her experiences at her former care home have taken their toll and have shortened her life, of that I am certain.
Long story but there has been collusion between the care home/social services and a financial deputy who was involved in order that a retrospective charge of approx £10,000 could be made – no explanation of this charge or why none of us were notified, despite being financial agents for my grandmother. Getting rid of a financial deputy is extremely difficult – the court of protection are loath to admit that she should never have been appointed in the first place, that the capacity assessment was falsified and that my grandmother’s former arrangements have been swept aside and her wishes completely ignored. I would advise anyone not to wait until it’s too late: sort out a POA before it becomes necessary as once the court of protection become involved, it really is a case of the State taking over completely.
NHS England are just as corrupt – they’ve attempted to block our complaint about the GP (who falsified a COP3 form and also diagnosed my grandmother with terminal cancer, without informing her family or sending her for tests)
They said that my grandmother lacked capacity to consent to her family making a complaint on her behalf – despite the fact we had her written consent, witnessed by a grade G nurse.
They were more interested in shutting us down, than in what had actually happened to my grandmother and the GP’s actions.
I’ve had to persist for 3 months and it is only the intervention of her current GP that has forced them to instigate an investigation
I’ve received an abject apology from a “director” who says that she has spoken to the manager and is now reassured that she has learnt from this and that it will not happen again – the question is, how many times has it happened previously, but because the complainant was perhaps not as persistent (bloody minded!) as I, they accepted NHS’s refusal to investigate.
Following NHS’s England’s logic, a person who may lack capacity has absolutely no way of making a complaint about their treatment – unless they have given POA to someone. It is just madness
As a family we’ve never had any involvement with social services – this has opened our eyes and made us realise that it’s all about profit, not what is best for the person that is paying for their own care.
Thanks for listening
LikeLiked by 2 people
Thank you very much Lisa for sharing and for this detailed account. I am sure others will find it useful and informative. I am extremely sorry for the troubles you have had. With best wishes.
LikeLiked by 1 person
It’s interesting. Local Authority safeguarding teams are always the lead agency for these types of investigation. The law only allows for the CQC to investigate complaints concerning people detained under the Mental Health Act. Of course, the CQC should not have said that they conducted an investigation themselves.
The CQC came into being with ‘Labour’s bonfire of the quango’s’ – they had made too many and wanted to reduce the overall number.
Controversies where providers have felt unfairly treated by the CQC? Find any inspectorate (OFSTED, HMIP etc.) where some of those inspected do not feel the inspection or report are fair.
The CQC is far from perfect but the senior management team changed in 2013, and the CQC has dramatically transformed since then (assisted with a reasonable budget which it never received when it was formed).
Dr Alexander, your comments are all negative. There is no balance at all. This comes across that you have an axe to grind and will dismiss any evidence that does not support your view. An organisation as big as the CC is unlikely to be all bad. NHS Trusts have good people/services/managers and not so good ones. Is there any chance that the CQC, with a comparable employee population could be the same? A number of your comments are based on your views with little evidence How do you know the CQC, an arms length body and independent commission has a political function? Their recent report ‘the state of care’ said social care was at a ‘tipping point’ – widely covered in the media and hardly supportive of government policy.
It is a shame that a Consultant Psychiatrist cannot see that the way they present their case looks far to one-sided and unbalanced, and does not seek to find solutions, just to identify (real or imagined) problems.
LikeLike
Thanks for your comments Steve. I think you’ve misunderstood the ‘complaints’ to which this article refers. These aren’t complaints about providers, but complaints about the CQC itself. The foundations of your critique are therefore a little wobbly.
I won’t reply exhaustively to your lengthy points – but I wonder if you’ve seen the latest report from the Centre for Welfare Reform which concludes that the CQC “misses abuse”, is “not effective”, “not responsive”, “doesn’t get relationships”, “costs too much”, “is hopelessly stuck” and so powerful that people in the sector are afraid to criticise CQC? The report can be found at this link:
Click to access whats-wrong-with-cqc.pdf
This follows on from a report by the Public Accounts Committee which also concluded that after 6 years, CQC was still ineffective.
I should point out that I have put forward solutions – such as abolishing the CQC and replacing it with something better.
LikeLike