Dr Minh Alexander retired consultant psychiatrist 25 April 2023
A secret within a secret within a secret.
After it was announced in January 2022 that HSIB would be stripped of its maternity investigations, I asked NHS England for a copy of the related King’s Fund review of HSIB culture and leadership.
When the King’s Fund review eventually arrived, after ICO interventions, it referred to “earlier reviews”.
When I asked NHS England for copies of those earlier reviews, only the internal 2020 Benson report on deficiencies of the HSIB maternity investigation programme was disclosed.
There had in fact been another highly significant investigation, by an external consultancy, Susan Newton Ltd. This took place in early 2021.
It was commissioned as a Freedom To Speak Up investigation by the central whistleblowing team at NHSE/I, to look into a whistleblowing case that is the subject of the current NHS England Employment Tribunal at Reading.
So NHS England tried to mislead me by omission. What’s new.
Susan Newton herself posted CV details of an investigation that she undertook in 2021 as follows:
March to June 2021: “Conducting a wide ranging investigation into whistle-blowing allegations relating to management culture and work practices. Findings and recommendations presented to the Board.”
An FOI request to NHS England on spending on Susan Newton Ltd’s services revealed a total spending of £140,595.70 in five years.
NHS England’s lawyers delayed my access to the Reading ET case bundle, and it was not until after several rounds of correspondence to the Tribunal and Tribunal Judge that access was finally facilitated on 24 April 2023, at which point I was finally able to see the Newton report.
For any journalists covering the case, the Newton report starts at page 622 of the ET bundle.
As might be anticipated, the Newton report was not flattering of HSIB leadership.
I will leave the media to pick up the bulk of the details.
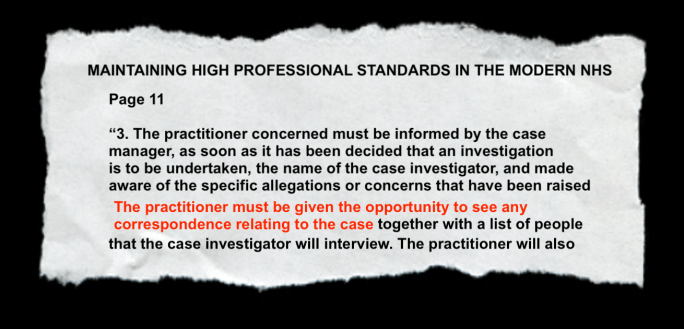
But in terms of the crucial whistleblowing governance, Newton found it unfathomable that the organisational response was to apply a grievance process to what was “clearly a whistleblowing complaint”.
Moreover, the decision to apply a grievance process was apparently not recorded.
But Newton suspected that senior managers influenced the decision.
Keith Conradi HSIB’s Chief Investigator received the claimant’s disclosure after disclosure to local managers was thwarted, and he was responsible for the central response.
Newton suspected that the grievance process was in part an attempt to keep the issues contained within HSIB:
“….there appears to have been an unwillingness to identify the complaint correctly and a desire to keep the whole process within HSIB”
Newton noted that a grievance process was applied despite advice by the HSIB Director of Corporate Affairs that it was a whistleblowing matter.
Newton expressed surprise that although the grievance process was very flawed, failed to follow the grievance policy and was full of omissions, it was deemed “very thorough”.
“The process deviated so far from policy that [the claimant] thought she had been referred to a different policy”
Newton pointed out in her report that this was despite Conradi reviewing the grievance documents himself, and thus omissions should have been evident to him.
“The Chief Investigator, as the Commissioning Officer, reviewed all the relevant documents so it is even more surprising that the investigation was deemed “very thorough” as it might have been assumed he would have easily identified the flaws given his role.”
Newton concluded that the whistleblower was not properly protected as a result of the organisational response.
Importantly, Newton took the claimant’s disclosures about conflicts of interest arising from HSIB maternity teams being regionally based very seriously and agreed entirely with her that this needed to be rigorously managed.
It is in the legal directions for HSIB that the independence of HSIB and its investigations must be maintained. Therefore, conflicts of interest would be incompatible with this legal obligation and breaches would be a matter that would fall under PIDA.
Newton’s professional response to the claimant’s concerns is in stark contrast to the response of local HSIB managers, who had told the claimant that she should not disappear down “rabbit holes” and who had sent emails discrediting her, including derogatory remarks about her “fixated” and “unstable” mental state.
It seems strange that NHS England was willing to pay good money for the advice from Newton and acted upon it by commissioning the King’s Fund external review of culture and leadership at HSIB, a further significant expense, but now apparently rejects the notion that the whistleblower was a whistleblower.
In an amended ET3 (Grounds of Resistance) of 31 January 2022 and throughout cross examination of the claimant. NHS England’s representatives have disputed that the claimant made protected disclosures:
“It is not accepted that the alleged disclosures at paragraph 2.1.1 of The Issues amount to protected disclosures.”
I have not finished by any means looking at the trail of disclosure correspondence in the bundle between the claimant and HSIB managers. I doubt that I will in the restricted time remaining. However, from what I have seen, I am perplexed by NHS England’s contention that no protected disclosures were made. Or perhaps I am not.
Importantly, in correspondence to Tom Grimes NHSE/I head of whistleblowing, Susan Newton reported to NHS England that during the course of her investigation, other HSIB staff also started whistleblowing to her.
Importantly, Newton also recommended at the end of her investigation that there should be an independent investigation into the claimant’s unresolved patient safety concerns:
“The safety concerns by [the claimant] should be investigated by a qualified and experienced person outside of the Maternity programme, and appropriate action taken internally and if appropriate, externally to satisfy all parties that this has been appropriately investigated and action taken.”
What happened to that?
The claimant does not believe her concerns were addressed and in fact has pointed out that NHS England seems to have lost some of the evidence relating to her clinical concerns.
NHS England made the claimant wait months before it gave her the Newton investigation outcome.
Susan Newton wrote to NHSE in September 2021 about this delay, to say she had “huge sympathy” for the claimant and that she could not believe that the claimant had not yet been told of the investigation outcome.
“I can’t believe she still hasn’t heard anything”
Prior to giving the claimant the Newton report outcome, Tom Grimes wrote an emollient email to KeithConradi Chief Investigator of HSIB:
Email dated 5 November 2021, headed “[Name of claimant] summary report”
“Dear Keith,
I hope your recovery is going well.
I am sure you will have been expecting to receive the attached finalised summary report regarding the [name of claimant] FTSU case. It’s not been shared with anyone else at HSIB but we will need to share it with [claimant] very shortly.
I understand you are due to speak to Aidan today, and so you will have an opportunity to discuss it with him.
If you can confirm receipt, I will then share the password with you, or you can obtain it from Aidan.
With very best wishes,
Tom”
The tone of the NHSE correspondence to the increasingly distressed claimant is in contrast to this.
Email dated 26 November 2021, headed “Confidential – Susan Newton’s report” from Tom Grimes to the claimant
“Dear [Claimant],
Thanks for your email. I will respond to your email in order.
- Yes. This is a summary of Susan’s report.
- Sophie Ellis was an NHS Improvement legal director at that time. To be clear, referencing her role does not waive legal privilege in respect to any legal advice she gave. There was no formal escalation process to the NHSI Legal Team because HSIB HR and Legal is separate to NHSE/I. Sophie did not formally oversee HSIB HR matters but was available for ad hoc advice. It was in that way that your case was raised with Sophie. Sophie responded to one brief, high level query and no further input was sought by HSIB. HSIB continued with the conduct of the case. It is not clear that Sophie’s advice was interpreted accurately by HSIB staff.
- The delay was clearly regrettable and there is a limit to how much explanation I can provide. However, the report’s findings impacted on others and as I explained on 28 April, before we could release the summary report to you we needed to consider carefully how the findings of the report were shared with you and others. Recognising the impact on you of the delay, I informed you on 28 May that, in relation to each of element of the ToR of the FTSU investigation, the investigation found flaws in handling of your grievance and in responding to the original concerns themselves.
I hope that’s helpful.
With best wishes.”
What is quite obviously missing in the NHSE response is the fact that the claimant was not immediately told of Susan Newton’s recommendation that her unresolved patient safety concerns should be independently investigated.
Patients. What are patients? What do they look like, these things called “patients”? Has anyone seen one?
But as all whistleblowers, patients and families know, the D’s prevail.
Delay, deny, defend.
And of course, the most important names are usually kept out of the picture.
I have written to Dr Aidan Fowler NHS England National Director of Patient Safety in England and a Deputy Chief Medical Officer at the Department of Health and Social Care, who oversaw this matter, and also oversaw the King’s Fund review and the HSIB maternity schism.
I have asked him more precisely what elements of the Newton report’s findings were accepted by NHS England, with reference to NHSE’s current rejection of the claimant’s protected disclosures.
I have also asked for clarification of whether NHSE acted upon Susan Newton’s recommendation that the claimant’s unresolved patient safety issues should be investigated.
LETTER TO AIDAN FOWLER
BY EMAIL
Dr Aidan Fowler
National Director Patient Safety, NHS England
Deputy Chief Medical Officer, Department of Health
25 April 2023
Dear Aidan,
Action upon 2021 Whistleblowing investigation into Healthcare Safety Investigation Branch/ NHS England by Susan Newton
As you will be aware, this investigation took place in the Spring of 2021 but the affected whistleblower was not provided with a summary report by NHS England until November 2021.
This is of huge concern because one of the most important recommendations from this report was that an external investigation was required into the whistleblower’s unresolved patient safety concerns. Susan Newton recommended:
“The safety concerns by [the claimant] should be investigated by a qualified and experienced person outside of the Maternity programme, and appropriate action taken internally and if appropriate, externally to satisfy all parties that this has been appropriately investigated and action taken.”
As a far as I can see, this has never been acted upon, or if has been acted upon, it has been done secretly and without involving the whistleblower, against the terms of the recommendation.
The whole safety of the HSIB maternity investigation programme has since come into serious question and has had to be remodelled nationally.
I should also point out that NHS England has been improperly hiding the existence of this 2021 whistleblowing investigation and misled me by omission in an FOI response, which adds to the impression of suppression.
The report is now in the public domain at page 622 of the bundle of an Employment Tribunal claim currently being heard at Reading, and shows shocking governance failures in a safety agency.
Susan Newton the investigator clearly accepted the validity and seriousness of the whistleblower’s public interest disclosures and made a slew of recommendations flowing from this, which as far as I can see NHS England broadly accepted in that it commissioned a review of HSIB’s culture and leadership as advised.
However, NHS England has since reversed and has claimed to the Employment Tribunal that the whistleblower has NOT made protected disclosures, which seems a disturbing position. I have been observing the Tribunal proceedings and have been very surprised by some of NHSE’s barrister’s contentions, such as an assertion that a concern about tampering with medical records is not a qualifying disclosure under UK whistleblowing law. This implies that NHS England does not consider tampering with medical records is unlawful, even though an investigation of records falsification by a predecessor body in 2012 determined that tampering breached a number of legal obligations. There are also other ways in which medical records tampering may be relevant to UK whistleblowing law.
NHS England might wish to review how it instructs counsel generally, but in particular in the conduct of whistleblowing cases, given its recent defeat in Cox v NHSE. Also the Care Quality Commission’s recent defeat in Kumar v CQC, where CQC defamed the whistleblower repeatedly.
It tends to have a chilling effect on the workforce and is contrary to national Freedom to Speak Up strategy to see these cases play out in this way.
I would be very grateful for the following clarification:
1. Which of the findings of the 2021 Susan Newton whistleblowing investigation report did NHS England accept?
2. Which of the findings of the Susan Newton whistleblowing investigation report did NHS England reject?
3. What follow up actions did NHS England take pursuant to the Susan Newton whistleblowing investigation report?
4. What actions did NHS England take in relation to Susan Newton’s recommendation that NHS England arrange an external investigation into the whistleblower’s unresolved patient safety concerns, as per the terms above?
5. If NHS England did NOT undertake an external, independent investigation into the whistleblower’s unresolved patient safety concerns, what was the recorded decision for this, assuming a decision was recorded?
I copy this to Mr Vineall at the Department of Health whom I understand has oversight of these matters and to the relevant parliamentary committees.
For parliament’s information, I should point out that in a five year period including the 2021 HSIB whistleblowing investigation, NHS England indicated via FOI that it paid Susan Newton Ltd over £140K for several pieces of complex Human Resources work.
One imagines from the recurrent commissions that NHS England was satisfied with the quality of the work commissioned.
Many thanks,
Minh
Dr Minh Alexander
Retired consultant psychiatrist
Cc William Vineall Director of NHS Quality, Safety, and Investigation DHSC
Public Accounts Committee
Health and Social Care Committee
UPDATE 27 APRIL 2023
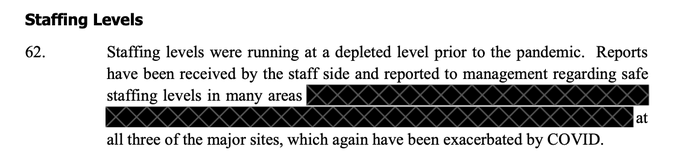
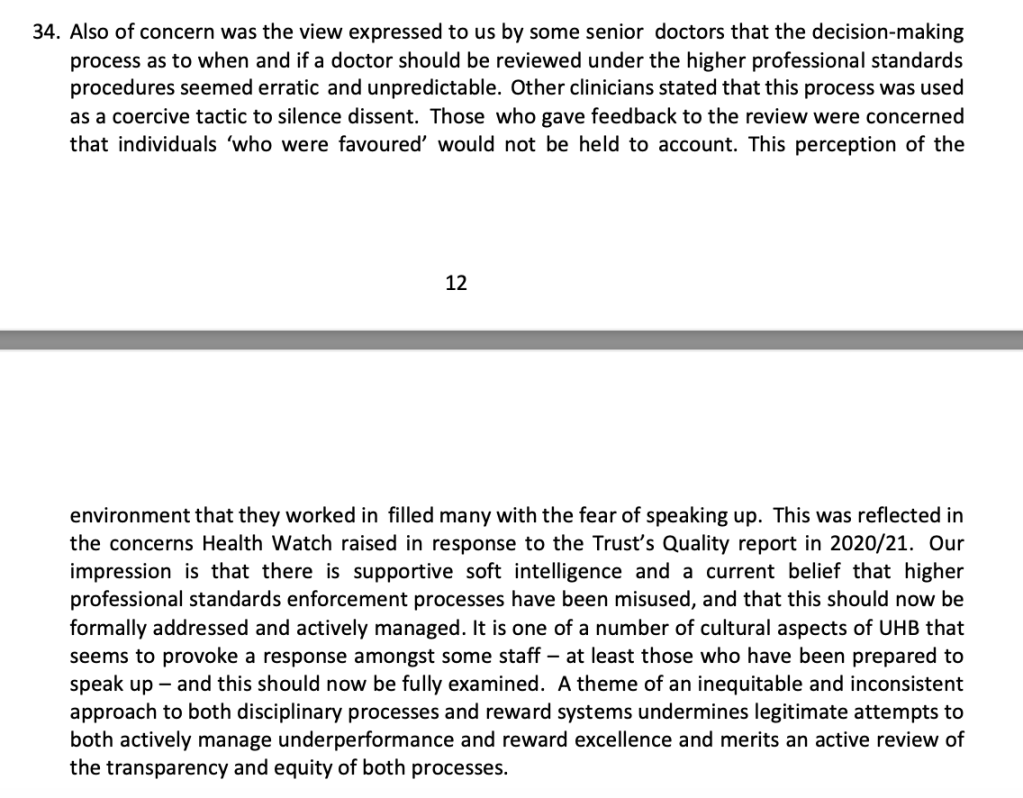
I have today shared disclosed documents from the ET which reveal previously withheld data from the Benson review. The un-redacted extracts from the Benson report show reports that the HSIB senior team told the HSIB workforce there would be a “threat to jobs” if the maternity report backlog was not cleared. Staff told Dr Dawn Benson and her co-reviewers of related pressure to churn out reports. Some left HSIB because they felt investigation integrity had been consequently been compromised, but feared reprisal by HSIB senior management after they returned to clinical roles. Issues about staff inability to challenge HSIB senior managers were identified.
If Keith Conradi HSIB Chief Investigator had ultimate responsibility for the undue pressure on HSIB maternity investigators to churn out investigation reports without due regard for safety, he should have recused himself from dealing with the claimant’s whistleblowing case about these issues.
RELATED ITEMS
Prescribed Persons or the Pretence of PIDA. How UK whistleblowers are ignored
HSIB whistleblowers and the Secret King’s Fund Fact Lite report
More secret HSIB reports and failures of HSIB maternity investigations
Replacing the Public Interest Disclosure Act (PIDA)
What could a new whistleblowing law look like? A discussion document