| Please sign and share: Replace weak UK whistleblowing law, and protect whistleblowers and the public |
By Dr Minh Alexander NHS whistleblower and former consultant psychiatrist, 8 August 2020
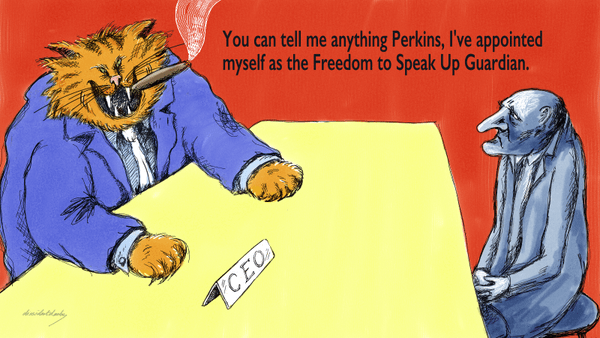
| Summary: Due to poorly designed systems and poor culture, NHS employers are able to treat healthcare workers unfairly with impunity. Oversight bodies allow this to continue by turning a blind eye. The disempowered status of NHS frontline workers and the consequent lack of genuine freedom to speak up is a safety issue. An example of very poor HR practice is given regarding Harrogate and District NHS Foundation, as found on a review of trust culture and leadership by Deloitte. The staff mistreatment at Harrogate is examined through the case of Dr Julian Campbell, consultant anaesthetist who suffered a surreal six year ordeal and unofficial restriction of his practice. He informed the General Medical Council, Care Quality Commission and National Freedom To Speak Up Guardian about the poor HR practices at Harrogate and their impact on patient care, but they deflected his concerns. Of very serious concern, after Dr Campbell sought help from the National Guardian’s Office, he later discovered that the National Guardian contacted the local trust Freedom To Speak Up Guardian without his permission. This was despite this person being married to the Medical Director about whom he had raised concerns. This is additional evidence raising serious questions about the impartiality of the National Guardian’s Office and the degree to which it may pose a risk to NHS whistleblowers. To genuinely protect whistleblowers, UK whistleblowing law needs to be reformed and ineffective schemes should be replaced with robust enforcement infrastructure. |
Introduction
Many cases over many years have shown that NHS doctors have few rights when their organisations take against them.
Doctors are therefore dependent on a post code lottery, in which some fare well. But the lottery is determined by the competence and integrity of local managers, and whether such managers choose to abuse disciplinary processes for ulterior motives or out of incompetence.
This injustice has serious implications for patient safety because of its effect on culture and workforce confidence.
Harrogate’s restriction of a doctor’s practice
Multiple staff have raised concerns about Harrogate’s culture.
One of these is Dr Julian Campbell, consultant anaesthetist, who experienced the nightmarish disempowerment which can follow accusations about medical competence.
Allegations were made about Julian Campbell’s clinical practice in 2015 after twenty years as a consultant with no previous such concerns raised against him. Restrictions were placed on his practice. A long, very stressful saga followed for him and his family. He was referred to the National Clinical Assessment Service (NCAS). His Royal College found there were no safety concerns with his patient care, but six months training was recommended, which he successfully completed based on advice from his Medical Defence body. But irregularly, he remained banned from working unsupervised on call and in the trust’s ITU on the grounds of “confidence”.
Alongside this, Dr Campbell raised concerns about the Deputy Medical Director’s repeatedly antagonistic behaviour towards him and his concern that this sometimes seriously affected patients’ care. He raised these concerns with the trust personnel director and his clinical lead.
Dr Campbell and his wife Judith later made representations to regulators – the General Medical Council and Care Quality Commission, and to Henrietta Hughes the National Freedom to Speak Up Guardian, raising concerns about unfair treatment, bullying, ageist treatment (they say that at one point, he was asked if he was too old to do on call), irregular handling of evidence by senior trust doctors and the trust’s failure to properly address the issues of patient safety raised by Dr Campbell.
For example, Judith Campbell informed the GMC of the following events:
“Mrs Campbell told us about an incident referred to as the ‘sentinel case.’ This case concerned a patient whom Dr Campbell had anaesthetised in May 2014 and was discussed at an ITU morbidity and mortality meeting (‘M&M’ meeting) on 14 May 2015. The patient had undergone a laparotomy on [date redacted to avoid patient identifiability, but the surgery had taken place one year previously]. Mrs Campbell explained that two doctors inaccurately presented that patient’s case to the M&M meeting without any prior communication with the professionals who had provided care for the patient. The errors in the presentation were such that Dr Campbell did not even recognise the patient when the case was presented. Mrs Campbell explained that the patient in the sentinel case was presented in such a way that prima facie, the consultant anaesthetist who had treated the patient had failed to undertake a number of basic actions and the failure had contributed to the patient’s death. However, Mrs Campbell says that in reality, the patient was palliative and subsequently died on ITU.
The day after the M&M meeting, the Deputy Medical Director told Dr Campbell in an email that he was the consultant anaesthetist who was responsible for the treatment and imposed supervision upon Dr Campbell, preventing him from being solely responsible for anaesthetising patients in category ASA 3 and above until he had undergone additional training. Dr Campbell was also prevented from working unsupervised on ITU.”
An important concern that Julian Campbell raised was that the trust’s Freedom To Speak Up Guardian, a doctor, was married to the then Medical Director David Scullion, with arising of conflict of interest.
In Julian Campbell’s case, this made it impossible for him to raise a concern about the actions of trust medical managers with any sense of safety and security. Indeed, he received an email on 23 November 2018 from the Freedom To Speak Up Guardian commenting on this issue:

Dr Campbell subsequently flagged the conflict to the trust Chair and the then chief executive. He reports that they refused to accept that any conflict existed. The Freedom to Speak Up Guardian continued in her role despite his concerns.
Harrogate’s management
Harrogate’s previous chief executive until her retirement in March 2019 was a medic, Dr Ros Tolcher. Dr Campbell was told by her successor that she had hired Deloitte to undertake a review of trust culture.
In April 2019 Dr Tolcher was succeeded by Steve Russell, formerly NHS Improvement Executive Regional Managing Director London, (who incidentally oversaw the very late establishment of NHS Improvement’s useless NHS whistleblower employment support scheme).
Under Steve Russell’s tenure, the Deloitte review commenced in August 2019. Deloitte has a very poor history of whitewashing, such as at The Royal Wolverhampton NHS Trust and at Derbyshire Healthcare NHS Foundation Trust.
But even Deloitte, whilst emphasising positives, could not fail to make some damning findings against Harrogate’s management.
These are some of Deloitte’s critical findings, including perceived conflict of interest regarding the Harrogate Freedom To Speak Up Guardian being married to the Medical Director, and astonishingly heavy handed application of staff capability procedures. The latter included irregular “informal capability plans” [consistent with Julian Campbell’s experience] without prior communication, sometimes denying staff representation during such processes.
| Independent assessment of leadership and culture at Harrogate and District NHS Foundation Trust and Harrogate Integrated Facilities Management
“A significant feature of our work was the number of both medical and nursing staff who reported apprehension or fear regarding the incident reporting and investigation approach in place at the Trust. Staff specifically cited the Complaints and Risk Management Group (CORM) as a source of fear, either as a result of personal experience or reputation. This was particularly (but not exclusively) felt to be an issue for the medical staff we spoke to. It is unusual for us to receive such consistent feedback that a single governance entity is a source of trepidation, as a result it would appear wise to revisit the governance structures around patient safety and particularly in relation to CORM.” “The Freedom to Speak Up arrangements in place at the Trust were frequently commented on by the medical staff interviewed as part of our work, with many feeling that current arrangements presented an actual or potential barrier to openness. Whilst no individual questioned the integrity of the FTSUG (who was frequently described as accessible, approachable, compassionate and helpful), our view is that the potential conflict of interest that exists under the current arrangement is such to act as a deterrent to some who may wish to raise concerns.” “We have been unable to undertake targeted work to evaluate the views of minority or hard to reach groups of staff due to the lack of diversity and inclusion structures, forums and arrangements in place at the Trust. In our experience not having such arrangements in place is unusual, as most NHS Trusts have implemented and well established such structures. Whilst some racist attitudes were present in free text comments in response to the survey of HIF staff, we had no direct issues raised with us regarding equality and diversity related bullying during our work.” “Whilst it is not unusual for some staff to criticise the responsiveness or level of service provided by corporate services during our reviews, human resources support at HDFT was frequently criticised by staff during our work. The HR department was described variously as: · Providing variable advice (dependent upon who in the HR department a line manager spoke to); · Adhering rigidly and inflexibly to policy; · Being slow to act on issues, with cases dragging on in some instances for years; and · Leaving staff with a feeling that the HR position regarding behavioural issues is to try to “make them go away””. “We asked all those in line management positions what level of training and development they had received in relation to performance management, managing difficult conversations and resolving conflict. In all cases staff told us that they felt the current offer in place at the Trust in this area to be inadequate. Our work also found concerns regarding the quality of HR policy and procedure currently being applied at the Trust. For example, a number of staff described instances where they had been placed on an ‘informal capability plan’ by the HR team with no prior discussion or communication and that they had been denied any representation at the meeting scheduled to discuss and agree this plan. We understand that a programme of work to review HR policies has now been commenced.” “B.1 Medical Leadership A significant number of individuals raised concerns with us about the culture amongst medical staff at the Trust, in particular relating to medical leadership (it is important here to state that we received almost universal praise from staff in relation to the behaviour and leadership of the Clinical Directors). The staff reporting these concerns were of all grades and from a broad range of specialties. The concerns raised ranged from general issues about poor behaviour not aligned to the trust’s values, to direct accusations and descriptions of bullying and harassment. Of the 35 staff raising these concerns with us 26 explicitly used the term ‘bullying’ or ‘bully’ to describe behaviour and a number relayed instances where they felt they themselves, or others had been bullied. We have detailed some of the examples of bullying cited by staff in the full version of this report. A number of the staff we spoke to during our review referenced what they felt was the impact of the medical leadership culture upon engagement, openness and incident reporting from medical staff. These individuals explicitly stated that there was a negative impact upon the patient safety reporting culture at the Trust, to the extent that some behaviours were a deterrent to reporting.” “B.2 Radiology During phase 1 of our review a number of staff raised concerns about Radiology, either in general terms about Radiology as a department, or specifically regarding the practice and behaviour of individuals within Radiology. In all of these instances the concerns raised related to behaviours towards medical staff from specialties outside of Radiology when requesting scans. In phase 2 of our work we spoke to 14 members of staff from within Radiology directly, and a further 51 members of staff from Radiology responded to the survey based on the NHSI / Kings fund culture diagnostic tool. A number of staff raised general concerns with us about the culture in Radiology, referring to a department with a poor culture, and describing Radiology as being ‘unhelpful’, ‘unfriendly’ and/or obstructive department. Some staff from outside of Radiology (particularly the doctors in training who spoke to us) compared the department to others where they had worked, reflecting that they had not experience such problems requesting scans in other Trusts. In our own experience of undertaking leadership, governance and cultural reviews at NHS Trusts, we have rarely come across such strength of feeling about the approach of a Radiology department to requests. We found this issue to be mirrored within Radiology, where we found staff to use combative language when describing their department’s relationship with wider organisation. Triangulating this point, 60% of survey respondents within Radiology did not agree with the statement “the Trust values the service we provide”. “Finally, we found limited oversight and visibility of cultural and organisational development based assurance and indicators at Board and committee level. The Executives and Non Executive Directors interviewed reflected that this was a gap in the governance and assurance arrangements in place at the Trust. There is in our view scope to undertake work to strengthen this aspect of governance and provide greater opportunity to explore assurance on organisational culture at Board level.” |
Given that Deloitte previously minimised the very controversial Wolverhampton CEO’s proven whistleblower suppression as a mere matter of personal “style”, Deloitte’s report on Harrogate represents in relative terms, a very serious criticism
It is also relevant to note that in regards to Deloitte’s criticisms of the Radiology Department, David Scullion is according to the trust website a consultant radiologist and, he continues to work in that clinical role at Harrogate.
Deloitte’s review reported in February 2020. Its report summary dated May 2020 was published via the Trust board papers in June 2020.
In its response to the Deloitte review report, the trust has taken the upbeat tack that Harrogate is “already a great organisation”:
Nevertheless, the board papers indicated that the trust board undertook the following actions:
| “6. A summary of the actions agreed by the subcommittees is set out below.
a. Our Board will place culture and experience at the heart of its governance and decision making. This includes the creation of a people and culture committee, which will focus on culture and staff wellbeing, and the development and implementation of a more routine approach to identifying concerns about the culture and behaviours within teams. Our HR experts will focus on the proactive identification and resolution of issues, supporting first line leaders and teams to quickly address the underlying causes of behaviours that are not in line with our values. Finally, we have strengthened the leadership capacity of Harrogate Integrated Facilities through new appointments, and we have appointed a new medical director with specific leadership experience in culture and engagement who started in post on 15th June 2020. b. In order to better support staff the culture in which the incident reporting process sits will be reviewed, and the approach of CORM in particular, will be reformed. Support will be provided to users of Radiology and the Radiology team to agree a common vision for radiology at HDFT and standards of behaviour. The time taken to address concerns or poor behaviours will be reduced and a feedback loop to check for improvements will be introduced. OD support will be provided to Harrogate Integrated Facilities and external facilitation support to our radiology team, where a number of issues were identified will be commissioned to improve the experience of staff in Radiology and those who refer to it. Finally, our Freedom to Speak up Guardian arrangements have been reviewed and changes made from 18th June 2020. c. To further promote fairness, consistency and responsiveness the approach to concerns being raised, the application of HR policies, and the provision of advice which support these will be reviewed. Additional controls to recruitment have been put in place, whilst the overall process is reviewed. The pilot ‘first line leaders programme’ will be rolled out to all managers and leaders in HDFT and HIF and other development programmes will be aligned to this to ensure there is comprehensive support for managers. Our staff networks will be used to learn about the specific lived experience of colleagues from minority groups. Finally, our policy is being updated to specifically include how conflicts of loyalty and relationships between work colleagues should be managed. d. Formal investigations will take place focusing on behaviours in Radiology, into appointments identified as not meeting the required HR criteria and process in HIF and the reported culture of bullying in Estates. There will be an external assessment of the capacity and capability within HIF overall, and in more depth in Estates.” |
The trust has appointed a new Executive Medical Director who has replaced David Scullion on the board:
“We have recruited Dr Jacqueline Andrews as our new Executive Medical Director. She has significant medical leadership experience and has been appointed with specific objectives around the development of a positive culture. Jackie starts in June 2020.”
An internal email of 17 June 2020 by the board lead for Freedom To Speak Up showed that the Harrogate trust Freedom To Speak Up Guardian was stepped down due to the concerns about perceived conflict of interest. However, she has continued in her role as Deputy Director of Governance:
| “From: HDFT-UPDATE (HARROGATE AND DISTRICT NHS FOUNDATION TRUST) Sent: 17 June 2020 15:03 To: allusers; AllUsers Subject: Interim Freedom to Speak Up Guardian Arrangements Sent on behalf of Jill Foster, Chief Nurse, Non-Executive Director of Harrogate Integrated Facilities, Executive Lead for Freedom to Speak Up Dear Colleagues, Interim Freedom to Speak Up Guardian Arrangements HDFT is a values driven organisation; respectful, responsible and passionate. We promote the need to treat each other with kindness, civility and compassion. We want all our colleagues at HDFT and HIF to feel supported in their work, to experience civil and respectful behaviours, to feel that different perspectives are looked for and are welcomed, where there are concerns feel able to speak up safely and to feel that concerns will be acted upon swiftly and appropriately. The Freedom to Speak Up Guardians (FTSUG) have an important role for ensuring colleagues have a safe route for being listened to and supported in speaking up about patient safety, quality of care and their experience of working in our organisations. We have been reviewing our current Freedom to Speak Up arrangements to ensure there are no barriers to encouraging people to speak up. Currently we have two Freedom to Speak Up Guardians, Dr Sylvia Wood, Deputy Director of Governance and Shona Kerr, Health Visitor. From today, Sylvia will not continue in the role of Freedom to Speak Up Guardian. Sylvia was the Trust’s first Guardian and has worked tirelessly to ensure colleagues have been supported through difficult times, felt listened to and have had their concerns resolved. At the time Sylvia was asked by the Board to take up the role, it was known that she was married to the Trust’s Medical Director. Sylvia has undertaken the role with determination, passion and integrity, has always been open about this conflict of interest, and has been thoughtful in seeking to consider how to address such issues more broadly. However, it has become clear that despite Sylvia’s personal efforts, a marital relationship with a senior colleague is seen by some as a barrier to speaking up. On reflection, given the unique role of the FTSUG, the Board has decided that in order to be a FTSUG, it is important that there is no such conflict of interest. As David continues in a senior role in the Trust as a Consultant Radiologist it is not possible for Sylvia to continue as a FTSUG. She will therefore step away from this role from today and I would like to say thank you on behalf of the organisation for her dedication in developing this very important route for colleagues to bring forward their concerns. I am looking forward to continuing to promote a fair and just culture with Sylvia in her role as Deputy Director of Governance. I am delighted that Shona Kerr is continuing in the role of Freedom to Speak Up Guardian. In addition to Shona, two colleagues – Kath Banfield, Head of Nursing, and Alison Pedlingham, Head of Midwifery – have temporarily agreed to be Freedom to Speak Up Guardians. This is so we can all collectively agree to a permanent arrangement for Freedom to Speak Up Guardians. To help us decide our future Freedom to Speak Up structure I am asking all colleagues, if you wish to, to participate in a survey linked below: The survey will be closed on Friday 26 June 2020. Kind Regards, Jill Foster Chief Nurse Non-Executive Director, Harrogate Integrated Facilities Executive Lead for Freedom to Speak Up” |
Inactive oversight bodies
Alongside the Deloitte review, the responses from GMC, CQC and the National Guardian to Julian and Judith Campbell’s concerns were typically deflective.
GMC
The GMC deemed that the concerns about trust medical managers were not at a threshold to bring them under GMC’s jurisdiction as fitness to practice issues, even though honesty was raised in some instances. GMC instead advised that they were matters for the trust to resolve.
The GMC stated in its final response of 23 October 2019 to Judith Campbell (ie. before the Deloitte review had reported):
“I am writing to let you know that having very carefully considered your request, an Assistant Registrar has concluded that there are no grounds for commencing a review of our decisions.
The reasons for the Assistant Registrar’s conclusion are explained in their decision, which is enclosed at Annex A. The Assistant Registrar has authority from our Chief Executive Officer to make these decisions.
I realise that it must seem cold and insensitive that we refer to the law and our rules when dealing with such a personal matter which has clearly been upsetting for both you and Dr Campbell. These are referred to only so we can fully explain what we can and cannot do, and why we have made the decisions we have.”
CQC
Although the CQC received Julian Campbell’s concerns in August 2018, it rated Harrogate “Good” overall and “Good” on the Well Led domain in March 2019, despite deeming the trust as “Requires Improvement” on Safety.

When later challenged with the evidence from the critical Deloitte review, the CQC stuck to its usual line of insisting that it does not investigate individuals’ concerns, and only undertakes generic inspection.
An email from CQC of 7 July 2020 to Julian Campbell stated:
“To clarify, we do not undertake investigations to resolve, prove or disprove the individual concerns a person has about their place of employment. The decisions our inspection personnel make are a result of evidence obtained and corroborated during and in between inspections. Even if CQC had concerns or found failings at the Trust in those areas raised by you, our role would be to drive improvements through issuing requirements or to take enforcement action.
From the records, I can see that the information shared with CQC was added to the central recording system alongside all the intelligence received about the Trust. In the planning of the inspection, I can again see your information has been taken into account and used alongside the views and experiences of other staff members.
I am satisfied that we have handled your information in line with our policies and procedures for whistleblowing. Clearly the Trust were aware of your concerns prior to our involvement. Our role is not to investigate the individual issues that whistleblowers may raise but to use our inspection powers to ensure that the Trust is meeting the fundamental standards. This was undertaken via the November 2018 inspection which included focus groups speaking directly with staff to gain their views on the culture in the Trust and saw that senior management were aware of the need to make improvements in some areas.”
Fit and Proper Person (FPPR) referrals have since been made to the CQC, but with little expectation that CQC will respond robustly.
The National Guardian
Julian Campbell first contacted Henrietta Hughes’ office on 21 August 2018 about his concerns with Harrogate’s managers and culture, and the conflict of interest surrounding the trust Freedom To Speak Up Guardian.
Henrietta Hughes’ Case Review & Governance Manager, Simon Pook, wrote back on 14 March 2019, implying that the conflict of interest with the trust Freedom To Speak Up Guardian had been resolved by the hiring of an additional Freedom To Speak Up Guardian:
“In response to the issue you raised concerning the trust Freedom to Speak Up Guardian and a possible conflict of interest, we have taken this matter up with the trust. As a result, to address the issue you have raised, the trust informed us at the end last week that they have now begun recruiting an additional Freedom to Speak Up Guardian to provide workers with an alternative source of support.
In respect of the other issues you describe in your referral, we are able to assist you to access support to raise this in your trust, for example should you wish to raise a formal complaint, or request an internal review of the handling of your case. While we appreciate that you may not wish support from the Freedom to Speak Up Guardian to do this, for the reasons you have given, we can help facilitate contact with others with responsibility for supporting workers to speak up, for example the organisation’s non-executive director.”
On 18 March 2019 Dr Campbell challenged this National Guardian’s Office (NGO) response and he expressed a serious lack of confidence in internal trust processes.
“To be offered support to raise the issues internally when I had understood that you would be an independent reviewer of the issues that I have raised is, quite frankly, devastating. Who will hold HDFT to account if the National Freedom to Speak Up Guardian won’t?”
In response, the NGO advised that it might consider a review of the trust, pending further enquiries:
“If we conclude…that the investigation was potentially flawed, we would undertake a review of how the trust responded to the issues you spoke up about to identify learning and improvement for the trust. Where we find evidence on such reviews of both speaking up culture, as well as process and policies that need improvement, we jointly agree actions to address this with the trust and our colleagues at NHS Improvement.”
Dr Campbell gave the National Guardian permission to contact NCAS and the trust Non Executive board lead for Freedom To Speak Up in order to make further enquiries about his case.
However, he later discovered that National Guardian in fact contacted the local Freedom To Speak Up Guardian about his case without his permission. He was told this by Steve Russell the trust CEO at a meeting on 11 June 2019.
He wrote in distress to the National Guardian’s Office on 13 June 2019:
“It has therefore caused me great distress to discover that the National Guardian did not contact the CEO, as your email indicated she would, but that she in fact contacted Sylvia Wood, who is now able to inform her husband.”
Following this challenge, the NGO wrote the next day to report that the National Guardian had spoken to the trust CEO that morning and:
“This discussion was encouraging. The CEO gave assurance to Dr. Hughes that the trust is keen to identify any learning and improvement concerning the matters you have raised with us. It was agreed that the trust will now contact you to discuss how to move forward on this, including agreeing a point of contact with you, with whom the NGO can liaise.”
But no National Guardian case review of Speaking Up at Harrogate has since been announced.
It is poor that the NGO initially accepted a governance bodge by the trust as “resolution” of the conflict of interest issues at Harrogate, instead of ensuring a truly safe solution was found.
It is especially worrying that the National Guardian contacted the trust Freedom To Speak Up Guardian about a case without permission, and without disclosing that she had done so. What does this say about the independence and impartiality of the NGO? How many other times has such communication taken place behind the scenes? The NGO already has little credibility with whistleblowers. Its failure to date to genuinely challenge vested interests has only strengthened the nagging impression that it was established to be a government PR tool. The Office was designed to be weak. If it fails to observe even whistleblowing basics such as respecting confidentiality, that would make it an active risk to whistleblowers and the public interest.
| Hypocritically in its most recent case review report published on 11 June 2020, relating to the Whittington Health NHS Trust, the National Guardian’s Office criticised the Whittington’s whistleblowing policy because of:
“Lack of information about how the trust would support and protect an individual’s confidentiality” |
Criminals have more rights than doctors
Julian Campbell and his family have endured six years of gruelling institutional processes, ending his long career as a public servant on a sour note. Whilst no oversight body has investigated what happened to him, the findings of the Deloitte review give credence to his concerns. Importantly, the review suggests that others have experienced mistreatment and arbitrary treatment, and that there is still potential for the pattern to continue.
Dr Campbell wrote to the NGO on 13 June 2019:
“ I have handed in my notice with the Trust. I reach the age of 60 on July 15th and my last day of service will be July 14th. My desire to leave not just HDFT but also medicine, and probably never return, is completely due to the maltreatment I have suffered. The ability of medical managers to behave badly without restraint seems to be complete.”
Reflecting on what happened to him, he comments:
“NHS safety is severely damaged by a culture of fear and the inappropriate promotion of those who are unsuitable to have power over others. With fear of reprisal by managers there is no freedom to speak up. In Harrogate the current national regulatory structures have protected those whose failings have led to poor patient outcomes and harmed those who have provided safe care.
Superficial initiatives are ineffective. Harrogate had a campaign of encouraging “kindness” in 2019. This will have limited effect on those who lack empathy.
I believe that the current national medical (and other) regulatory structures need to be changed, and that investigation of clinicians’ performance and conduct issues should be conducted independently, to avoid abuse of process by employers and managers with axes to grind.”
Dr Campbell’s wife Judith is a lawyer, who based on her professional experience commented:
“I really think we give more rights to our criminals than we do to our Drs”
The alleged serious mistreatment of NHS staff through overbearing HR process needs to be taken much more seriously. Staff are the NHS’ most precious resource. Doctors like Julian Campbell are trained and developed at great public expense. It is unacceptable and wasteful that there are insufficient checks against local management abuses. The NHS is a valuable public asset, not a private fiefdom, and Nolan principles of accountability should fully apply.
Alongside this, the ineffective National Guardian’s Office and NHS Freedom To Speak Up Guardian network should be replaced with genuine reform of UK whistleblowing law and related infrastructure.
The Deputy Governance Manager and former Freedom To Speak Up Guardian of Harrogate District NHS Foundation Trust, tweeting compliments to trust senior management in May 2019:

UPDATE 27 FEBRUARY 2021
An NHS Improvement investigation, albeit flawed, has upheld that the National Guardian’s Office breached Dr Campbell’s confidentiality:
RELATED ITEMS
- In another matter, based on reports received, I asked Harrogate if any concerns had been raised in the last five years about disrespectful or unlawful treatment of deceased trust patients’ bodies. On 21 February 2020, the Trust denied any such concerns:
“3. With respect to the reports that Savile was allowed to treat the bodies of deceased patients in a disrespectful manner at Leeds General Infirmary –
please advise if any concerns have been raised about any disrespectful, and or unlawful treatment, of deceased patients’ bodies at your trust in the last 5 years? No”
However, another roughly contemporaneous FOI request to the CQC revealed that the regulator had received a disclosure about the handling of a patient’s body:
“I can confirm that we hold one record from 2015 regarding one allegation of poor manual handling of a body and the staff concerned making inappropriate comments.”
The matter is inconclusive but a concern arises about whether the trust answered truthfully in February.
Unrelated to Julian Campbell’s case, I asked Harrogate under FOIA for data on trust grievances.
This too has since proved anomalous. The trust claimed to me that no individual grievances were upheld in 2017/18, but I now understand that Julian Campbell’s grievance was partially upheld.

Again, a concern arises about the truthfulness of the trust’s response.
2. In April 2020 Harrogate District NHS Foundation Trust staff whistleblew directly to the media over trust managers’ handling of PPE safety safety issues:
4. My Beautiful (Ministerial) Launderette: The National Guardian and Paula Vennells



Today 8.8 is the anniversary of my dismissal…
I thought on reading this report, I was reading about my case, the corruption and nepotism is so rife within the nhs, HR/WOD are corrupt to the core.
They destroy good nhs employees with no accountability for the inept, nepotism and lies.
LikeLike
You are absolutely correct, and, in respect of HR/WOD, once they are shown to have behaved in this way, they move on to other Trusts, where they have contacts who will offer them a job. Thus, the whole saga continues, the Web of deceit widens and bullying is not dealt with. When such people are appointed directors, and a complaint sent to the CQC, the FPPR should be initiated, but, don’t hold your breath. As far as the GMC is concerned, there is a regulator who fails to regulate. The GMC made a splash a while ago about how it dealt with bullies, yet when faced with evidence of bullying does nothing. Why? Because it would rather the tormentors act unfettered than bring them to book. It takes the easy option, whilst the bullied have to live with the consequences.
LikeLike
I am so sorry about your experience, Thanks for commenting and please look after yourself.
LikeLike
Thanks for commenting. I am extremely sorry to hear you had a really bad experience as well. All my best.
LikeLike
Dear Minh,
although I have been a victim of similar injustice it still distresses me to read about cases like this. We all owe you a debt of gratitude for continuing shine a light into this murky world. I have copied your summary paragraph which everyone should read especially those who care about the conditions of NHS workers and how that impacts on the safety of the services they are able to provide.
Thank you,
Tim
LikeLike
Increasingly, in our country, any pretence of democracy has been replaced by a culture of control and command. And the public is either aware and are, therefore, part of the problem or haven’t noticed and, consequently, cannot be part of any solution.
It’s an uncomfortable read. My heart goes out to Dr Julian Campbell – a long time to be ground down for no discernible reason. At least such victims know they are not alone.
I am surprised the NHS hasn’t invited Hugo Boss to design new uniforms. Only a matter of time I imagine.
Also, on looking upon the National Freedom to Speak Up Guardian’s office, why does – “Letting a hundred flowers blossom”- spring to mind? Because such an inspiring quote led to the self-identification and, therefore, destruction of the innocent?
Hopefully, I have totally misread the whole situation, and everything is beautiful, noble and for the best interests of patients and staff.
Thank you, Dr A. and good luck Dr Campbell.
LikeLike
This latest example is a repetition of what happened to Dr Kevin Beatt at Croydon NHS Trust in 2012. Just proves that NHS executives spend most of their time covering up for mistakes and elected politicians of all parties have done nothing to stop or prevent what they are doing in the interest of “self preservation” .
I shall be using your articles in evidence in proceeding as a patient who has also suffered injustice at the hands of two NHS Trusts for over 6 years Keep up the good work .
LikeLike
Dr Campbell endured vitriolic treatment at Harrogate, an excellent Doctor who in my opinion was targeted in a bid to cover up the failings of others. Sadly despite all of the positivity that Harrogate currently uses to “sugarcoat” the Deloitte findings, and let us not forget that this was merely a “Summary” disclosed to the staff, hence one can only imagine the contents of the full “never to be disclosed” report. They continue to treat others in the same manner as Dr Campbell. The toxic and chaotic mismanagement continues as those tasked with “investigating” spurious allegations against staff members are still allowed to continue their agenda. The Medical Director may have been removed from post but his toxic legacy continues. This has lead to some employees suffering from significant long term mental health issues. Just last week I heard about one Doctor at Harrogate hospital who recently attempted suicide such was his desperation. I would not be surprised if he is also enduring the same treatment as Dr Campbell, the rumours certainly appear to suggest this could be the case.
Yes, investigations into the culture are to take place, but we have to ask who are the investigators? and who is going to investigate the investigators? For many years Harrogate has chosen to keep all issues “in house” in a bid to cover up the toxic culture and suppress those employees who dare to raise any concerns. In the past “investigators” have been chosen from a cohort of senior staff who have been discreetly “briefed” on the “troublemakers” and the “required outcome”.
Is the new CEO really making changes?
Evidence suggests that he is trying, but it is all a little superficial, yes the Trust are attempting to make changes for the better, but sadly there remains a cohort of individuals who allow the culture to persist under the radar. There is a worrying refusal to acknowledge the effect that the vindictive behaviour of former senior medical management has had on individuals careers and health. These individuals are merely discarded as collateral damage, brushed under the carpet and hope they vanish! Would personal admissions of the Trusts failings to date and apologies to those wronged be too much? Sadly the answer is yes. Harrogate Hospitals corporate Image must not be tarnished and they will continue to silence those who dare to attempt otherwise.
LikeLiked by 3 people