By Dr Minh Alexander NHS whistleblower and former consultant psychiatrist 11 November 2016
Summary
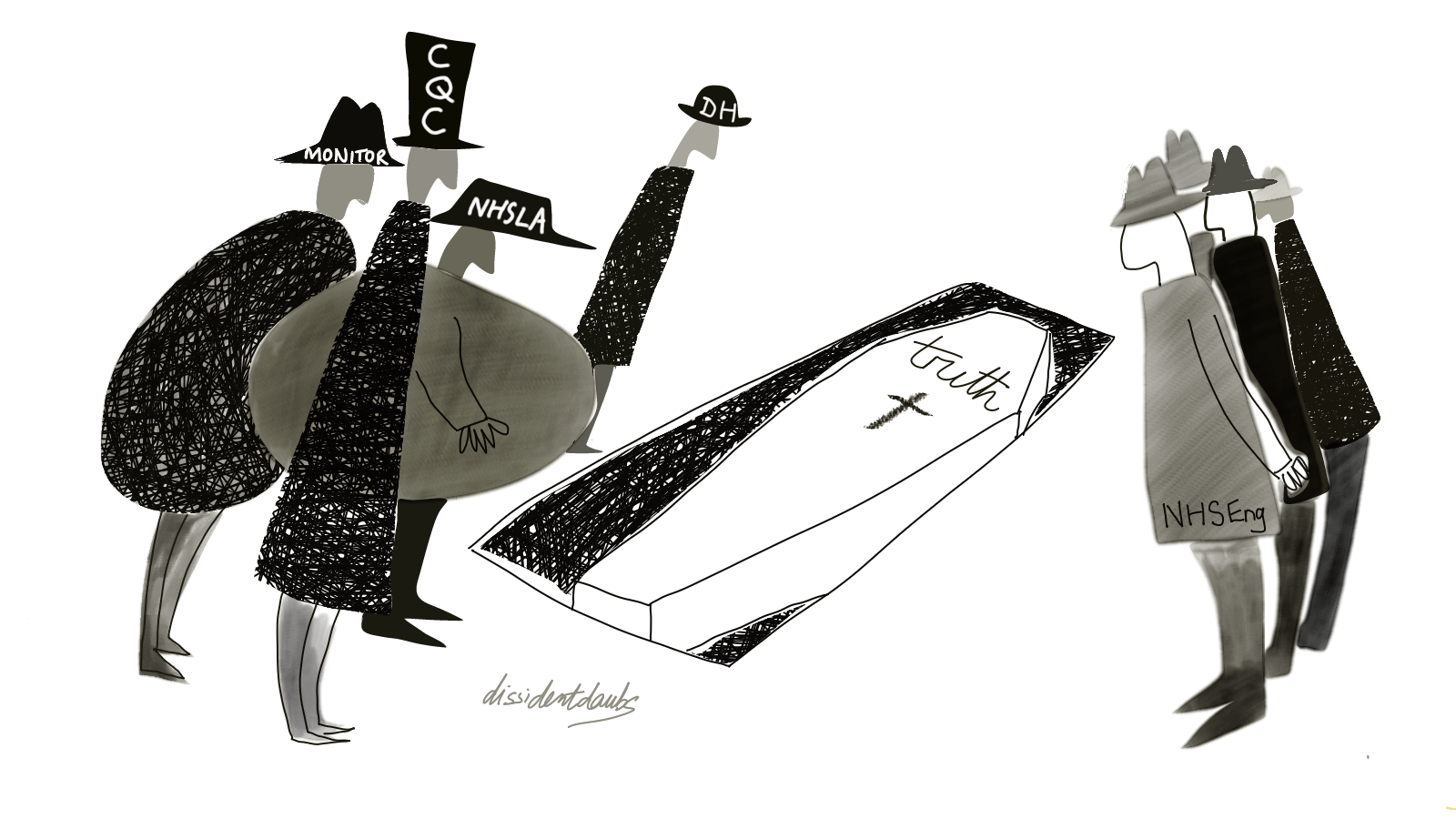
The Care Quality Commission’s purported transformation is a central plank in Jeremy Hunt’s claims of NHS reform and focus on patient safety. However CQC has not been revealing the full extent of unmet need and harm. [1] [2] Of great importance, CQC failed to reveal hundreds of deaths that had not been investigated by Southern Health Foundation Trust. [3] There have also been repetitions of Winterbourne View type failures [4] [5], despite new CQC leadership being installed in 2012. Two days ago, another Panorama undercover investigation into care failings emerged. [6] The CQC has also previously failed to report and act on coroners’ warnings about deaths [7], with little sign of improvement based upon a recent check. [8] The CQC has also given conflicting dates for when its memorandum of understanding with coroners was established. This has clouded issues of accountability. An analysis of coroners’ data shows that CQC has been sent 206 coroners’ Reports to Prevent Future Deaths (PFDs) since July 2013. Almost three quarters of the PFDs sent to CQC featured NHS organisations. However, there was published evidence of a CQC response in only nine (4.3%) of the 206 cases. Even when PFDs were directly addressed to CQC as a named respondent, only a fifth were apparently answered by CQC. The PFD reports reveal many serious risks to service users. Some shocking case examples are provided. It is troubling that CQC has not demonstrated a consistent response to the PFDs, or evidence of analysis of such serious matters. It is also evident that CQC inspection reports do not consistently and fully reflect coroners’ warnings. Greater transparency is needed about how CQC has used – or not used – vital intelligence from coroners.
Background
Coroners’ PFD reports (formerly known as Rule 43 reports) are warnings about risks to life, which are only exceptionally issued. The risks usually relate to the deaths reviewed by coroners, but other risks that are incidentally discovered are also reported. PFDs represent a small proportion of the many thousands of cases in which inquests are opened every year:
Table 1. Number all of coroners’ inquests opened in recent years:
| YEAR | NUMBER OF INQUESTS OPENED IN ENGLAND AND WALES |
| 2013 | 29,942 |
| 2014 | 25,899 |
| 2015 | 32,857 |
Source: Coroners’ statistics 2013, 2014, 2015 [9]
Only some of the PFDs are sent to the CQC, reflecting considerable concern by coroners. An effective regulator would reasonably be expected to investigate further.
In a report published in February 2015, CQC stated that it had reached a memorandum of understanding (MoU) with coroners in 2014, and that it had started receiving PFDs on deaths in any health and care settings, which it was passing to inspectors. [10]
In September 2015 after CQC was criticised for failing to respond to coroners’ warnings about care home deaths, the CQC changed its story and claimed that it only had a “proposed and drafted” MoU with coroners. [11]
When questioned this September about gross under-reporting of mental health PFDs [12], CQC claimed that its MoU with coroners had not covered the period 2014/15. [13]
When questioned last month by Disability News about the evidence of continuing failures to respond to coroners’ warnings about care home deaths, CQC maintained its claim that the MoU was not established until November 2015. [14]
Questions arise about why CQC has given conflicting accounts. Notwithstanding, PFD data is openly available to the public and CQC could easily have availed itself of coroners’ warnings about regulated bodies. [15]
Analysis and case examples
Review of published coroners’ PFD reports shows that 206 PFDs have been sent to the CQC about regulated bodies since July 2013. NHS organisations featured in 152 (73.4%) of the PFDS.
The PFDs related to 76 NHS providers, 46 social care providers – all private – and 11 private healthcare providers.
18.9% (39) of the PFDs were directly addressed to CQC and not just copied.
7.2% (15) of the PFDs were sent to CQC board members (13 to David Behan CQC chief executive, one to David Prior CQC Chair and one to Mike Richards, CQC Chief Inspector of Hospitals).
Table 2. Since July 2013, the providers that were most often reported to CQC by coroners were as follows:

CQC’s most recent inspection reports on 12 of the above 17 NHS trusts did not mention coroners’ PFDs, despite CQC being sent PFDs about these trusts prior to the issue of CQC’s inspection reports. Deaths were not mentioned at all in CQC’s reports about City Hospitals Sunderland NHS Foundation Trust and Leicestershire Partnership Trust. CQC’s report on troubled Brighton and Sussex University Hospitals NHS Trust noted the rate of some deaths in the local population but was silent on deaths of trust patients, besides commending end of life arrangements. CQC rated University College London Hospitals NHS Foundation Trust as ‘good’, without providing any data on deaths of trust patients and without mentioning that it had been subject to PFDs. Where CQC mentioned PFD reports, it stated that PFDs had been “submitted” or reported by trusts, which implies that CQC perhaps relies on trusts to tell it about PFDs. [16]
The full data on the coroners’ PFDs that have been sent to CQC since July 2013 can be found here:
cqc-pfds-since-july-2013-as-of-9-11-2016
Some individual failings by staff featured in the 206 PFDs sent to CQC but more often, coroners have described systems failings. Risk factors such as absence or inadequacy of policies and procedures, inadequate staff training, numbers and supervision, design flaws in premises and equipment, shortage of equipment, poor investigations and cover ups were described by the PFDs. Failures by providers to learn from repeated serious incidents and prior coroners’ findings were noted:
“This is a repetition of similar circumstances in a number of previous Inquests and I think the Trust needs to be assessed independently.” [17]
There were serious signs of service strain in the PFDs sent to CQC. For example after one death, it was revealed that the practice in one area was not to conduct Mental Health Act assessments when a need was identified, but to defer assessments until beds were available. In effect, serious risk and unmet need had been normalised. [18]
In total, there is only a published CQC response to nine (4.3%) of the 206 coroners’ warnings sent to CQC. There is no published evidence of a CQC response to 31 (79%) of the 39 PFDs that were directly addressed to CQC.
The PFDS that were apparently unanswered by CQC included grave cases. I give below four examples:
- Death of Jack Molyneux following care by Brighton and Sussex University Hospitals NHS Trust
https://www.judiciary.gov.uk/publications/jack-molyneux/
Mr Molyneux had Alzheimer’s dementia and needed all care, but did not receive it from the trust. The coroner reported that when he was discharged from hospital to a care home, the care home “immediately raised a Safeguarding concern on grounds of neglect”.
The coroner wrote in his report of 29 April 2016, copied to Jeremy Hunt, Simon Stevens and CQC:
“I believe this to be one of the most disturbing cases of sub-optimal care that I have come across recently, and I am not at all satisfied that this inquest will result in any effective action being taken which is why I am concerned to follow up this matter and to ensure that all those who should know about this situation are informed”
The subsequent CQC inspection report of 17 August 2016 failed to reveal that coroners’ PFDs had been issued, and did not give any data on the deaths of trust patients. On Safeguarding, CQC only noted that the trust had not met its own target for training:
“The trust had a safeguarding vulnerable adults and children policy, and guidelines were readily available to staff on the intranet and staff were able to access this quickly. However, safeguarding training for all staff groups was lower than the Trusts target.”
- Death of Patricia Cleghorn under the care of Birmingham and Solihull Mental Health Trust
https://www.judiciary.gov.uk/publications/patricia-cleghorn/
The Nursing Times recently reported on Mrs Patricia Cleghorn’s death shortly after being given a small dose (5mg) of diazepam, a sedative, by an unsupervised healthcare assistant. [19] She was under the care of the trust’s Home Treatment Team. This was because a need for hospital admission had been identified, but no mental health beds were available. The coroner concluded that she died of an intentional overdose and observed in his report of 25 July 2016:
“She was allowed to self-medicate drugs including amitriptyline and morphine, despite repeatedly stating she would take her life through an overdose”
This coroner’s PFD was addressed to the trust, the Department of Health, NHS England and CQC. These bodies were expected to respond to the coroner by 20 September 2016. There is no published response yet by any of these bodies.
- Death of Mohammed Chaudhury following care by King’s College Hospital NHS Foundation Trust
https://www.judiciary.gov.uk/publications/mohammed-chaudhury/
Mr Chaudhury required hospital care after a road traffic collision, initially in intensive care. He later developed several infected pressure sores whilst on a step down ward at King’s College Hospital. The coroner concluded that this was because he was not nursed on an air mattress and there had been insufficient staff to turn him as needed. He was transferred to a nursing home with “five pressure sores between grades 2 and 4, which were septic”. The coroner remarked that the pressure sores were “unusual in extent and severity” and concluded that they may have been a cause of death.
The coroners’s report of 20 August 2013 was addressed to Tim Smart then chief executive of King’s and Mike Richards CQC Chief Inspector. It was also copied to Jeremy Hunt. The deadline for responses was 1 October 2013. There is no published response from the trust, the CQC or the Department of Health.
- Death of Neil Carter under the care of Priory Roehampton
https://www.judiciary.gov.uk/publications/neil-carter/
Mr Carter was an inpatient at the Priory Roehampton, a private mental health hospital, when he took his own life. The coroner’s report of 5 March 2014 was addressed to the Priory Group and CQC. The coroner noted:
“There were gross failures in his care, notably the failure to perform basic observations followed by falsification of the record”
Despite this report of serious care failure and cover up, there is no published response by the CQC.
CQC’s inspection report of September 2014, from an inspection on 20 August 2014, made no reference to the coroner’s findings. Its inspection report did not mention deaths at all.
In short, many questions arise about the extent to which the CQC is acting upon and revealing evidence about serious risk to patients. I will submit the above data to parliament.
I invited the CQC’s comment three days ago, via its press office, on why there are apparently only a handful of CQC responses to coroners’ warnings and to explain its so far conflicting dates for its MoU with coroners.
I have not yet received a substantive response from the CQC at the time of writing, but will update this report if a response is provided.
REFERENCES
[1] How safe are NHS patients in private hospitals. Prof Colin Leys and Prof Brian Toft, Centre for Health and the Public Interest December 2015
https://chpi.org.uk/wp-content/uploads/2015/12/CHPI-PatientSafety-Dec15.pdf
[2] CQC Deaths Review: All Fur Coat. Minh Alexander
https://minhalexander.com/2016/09/25/cqc-deaths-review-all-fur-coat/
[3] Mazars report of Independent review of deaths with a Learning Disability or Mental Health problems in contact with Southern Health NHS Foundation Trust from April 2011 to March 2015
https://www.england.nhs.uk/south/wp-content/uploads/sites/6/2015/12/mazars-rep.pdf
[4] Orchid View Inquest: Home riddled by ‘institutional abuse’, BBC 18 October 2013
http://www.bbc.co.uk/news/uk-england-sussex-24579496
[5] Staff sackings and suspensions over poor elderly care. Alison Holt, BBC 30 April 2014
http://www.bbc.co.uk/news/uk-england-sussex-24579496
Old Deanery whistleblowing proves system does not work, says campaigner
[6] Care Home closed after BBC investigation, Natasha Swift, St. Austell Voice 9 November 2016
http://www.staustellvoice.co.uk/news/73/article/5971/
[7] Elderly people put at risk as watchdog fails to act on warnings of ‘fatally negligent’ care homes
[8] Care home deaths and more broken CQC promises
https://minhalexander.com/2016/10/08/care-home-deaths-and-more-broken-cqc-promised/
[9] Coroners’ statistics for England and Wales 2013,2014,2015
[10] CQC Mental Health Act monitoring report 2013/14 and associated press release 5 February 2015
http://www.cqc.org.uk/content/new-report-published-looking-use-mental-health-act-201314
[11] CQC press release 3 September 2015
http://www.cqc.org.uk/content/cqc-response-story-independent
[12] Letter to David Behan CQC chief executive 9 September 2016
[13] Letter from Paul Lelliott CQC Deputy Chief Inspector 26 October 2016

[14] Care watchdog ‘fails to follow up on coroners’ warnings. John Pring. Disability News, 27 October 2016
http://www.disabilitynewsservice.com/care-watchdog-fails-to-follow-up-on-coroners-death-warnings/
Statement by Andrea Sutcliffe CQC Chief Inspector 27 October 2010:
“We have previously acknowledged that our handling of reports from Coroners has not been sufficiently effective which is why we carried out an internal review in 2014, introduced new procedures in 2015 and established a formal agreement with the Coroner’s Society in November 2015.”
[15] Chief Coroner’s published data on Reports to Prevent Future Deaths
https://www.judiciary.gov.uk/related-offices-and-bodies/office-chief-coroner/pfd-reports/
[16] Summary table of information about PFDs in CQC reports on the providers that were most often reported to CQC by coroners:
[17] Report to Prevent Future Deaths. Kathleen Dixon:
https://www.judiciary.gov.uk/publications/kathleen-rosemary-dixon/
[18] Report to Prevent Future Deaths. Rohan Fitzsimons.
https://www.judiciary.gov.uk/publications/rohan-fitzsimons/
[19] Trust admits neglect after patient died when unsupervised HCA administered drug, Rebecca Thomas Nursing Times 3 November 2016

I thank you for this catalogue of horrors. What a pity we no longer have investigative journalists to, not only report these – let’s be honest about this – unlawful deaths – but to hold those responsible to account and shame all involved.
Nor, apparently, do we have effective MPs or, institutions worthy of the name, to take a real interest.
I wonder who gains comfort from learning that the CQC have assured us that they will be busily occupied collating these reports? (They may not have time to actually action anything relevant I would guess).
Thank you, Dr A. Have a good weekend.
LikeLiked by 1 person
Thanks zrprayder. I find it all very surreal. Whistleblowers have a lot to thank the media for, but press independence seems increasingly threatened by a shrinking pool of powerful corporate owners. We plod on. You have a good weekend too. BW Minh
LikeLiked by 1 person
Thank you for this info Minh and Remembrance Day is a great date to ‘go public’ I have my meeting with CQC Dr Paul Lelliott on Monday and intend to use this info to inform me. I am traveling in with my sister (but staying with her this weekend. Thank you again…..and not too much to print off either! :o)
LikeLike
Have a good weekend too xx
LikeLike
Thank you Dee. Hope the meeting next week is helpful to you. All best, Minh.
LikeLike