Dr Minh Alexander, retired consultant psychiatrist 3 May 2025
This is a brief follow up to my last post, in which I reported on issues surrounding a dangerous shortage of NHS mental health beds in England.
The issues are set out in detail in that report. The issues relevant to mental health crisis services can be summarised as follows.
Mental health beds have been relentlessly cut despite protests by patients, families, professionals and Royal Colleges.
Politicians and senior NHS leaders have claimed that there has been investment in community services to compensate for bed loss, and policy has been devised to reduce access to beds.
The introduction of a gatekeeping function by community-based mental health crisis resolution teams has been key, and has in some instances inappropriately and unsafely blocked access to inpatient care.
The services offered by crisis teams have been flourished by politicians and senior NHS leaders as part of the justification for cutting mental health beds, but crisis teams are neither sufficiently resourced nor safe. NHS crisis services currently lack crucial elements needed for fidelity to a recommended model of safe and sufficiently intensive care.
An aspect of these safety failures has been failure of risk assessment and management. The failures are reflected in repeated coroners’ Prevention of Future Deaths reports.
Crisis teams were mandated by The NHS Plan 2000, with a requirement for establishment by 2004.
By 2014 the National Confidential Inquiry into Suicides and Homicides by People with Mental Illness (NCISH) warned that work was needed on the safety of crisis services. Crisis teams accounted for about twice as many suicides as inpatient services (and the running total suggests that they still do).
NCISH also questioned the practice of using crisis teams to facilitate early discharges from hospital. However, the practice has continued, and is in fact required by NHS England guidance on mental health bed management:
“A review of all inpatients individually, to agree on the appropriateness of their continued stay in light of current and predicted levels of activity, and consider whether any of them could be discharged early with increased follow-up by community mental health teams.”
Moreover, NCISH found in 2014 that 43% of suicides under crisis teams were by patients who lived alone.
NCISH advised that providers should be cautious about treating such higher risk patients under crisis resolution/ home treatment teams, and should review their entry criteria for such services.
“CR/HT [Crisis Resolution/Home Treatment] may not be suitable for patients at high risk or those who do not have adequate family or social support: services should review their criteria for its use.”
NCISH advised that more suicide prevention work was needed with regard to crisis teams:
“CR/HT should be a priority setting for suicide prevention in mental health services.”
Failure to improve since NCISH’s 2014 warning
I asked the National Confidential Inquiry about repetition of its 2014 analysis of the social circumstances of people who died by suicide under the care of crisis teams, to see whether NCISH’s advice had been implemented and whether there had been a drop in the proportion of suicides by people who lived alone.
The Inquiry advised that the analysis was repeated in the four following years up to 2018. This showed no reduction in the proportion of patients who were living alone when they died of suicide under crisis service care:
| Period | Page of annual report | Proportion of CR/HT suicides in patient who lived alone |
| Report 2014 (2002-2012 data) | Page 42 | “666 (43%) CR/HT patients lived alone” |
| Report 2015 (2003-2013 data) | Page 27 | “In 795 (43%) the patient lived alone.” |
| Report 2016 (2004-2014 data) | Page 29 | “In 833 (43%) the patient lived alone.” |
| Report 2017 (2005-2015 data) | Page 36 | “In 883 (44%) the patient lived alone.” |
| Report 2018 (2006-2016 data) | Page 55 | “In 834 (43%) the patient lived alone.” |
In addition, data for the period 2012 to 2022 also suggests that this lack of improvement has persisted. Between 2012 and 2022, 841 patients who lived alone died by suicide under the care of crisis teams:
“Based on this 2012-2022 dataset, there were 1,970 patients under CRHT services in England who died by suicide, of whom 841 (44%) were living alone.”
This is the FOI response by the National Confidential Inquiry.
Taken with the NCISH 2014 data for the period 2002 to 2012, when there were 666 crisis team patients who died by suicide and lived alone, a total so far of 1507 crisis team patients who died by suicide lived alone.
Questions arise about what actions have been taken by NHS England and the Care Quality Commission to ensure learning from the National Confidential Inquiry’s warnings. Also, if no effective action was taken to reduce the risk of suicide by patients under crisis teams, was this due to inefficiency or unwillingness to impede the political drive to cut beds?
RELATED ITEMS
1) Waiting “for the grown ups to arrive”. Dangerous shortage of mental health beds, the government’s deflection of coroners’ warnings and normalisation of bad practice by NHS England A lengthy but indexed report with data, on the wilful blindness of politicians and NHS England to the harm caused by unsafe cuts to mental health beds.
2) NHS England’s handling of independent investigations on mental health homicides A report with data on how NHS England fails to ensure learning from mental health homicides. As part of this, NHSE has not shown appropriate accountability and there is opacity on how only a proportion of mental health homicides that are eligible for independent investigation are actually independently investigated. Access to mental health services, including to mental health inpatient treatment, has been a factor in these homicides.
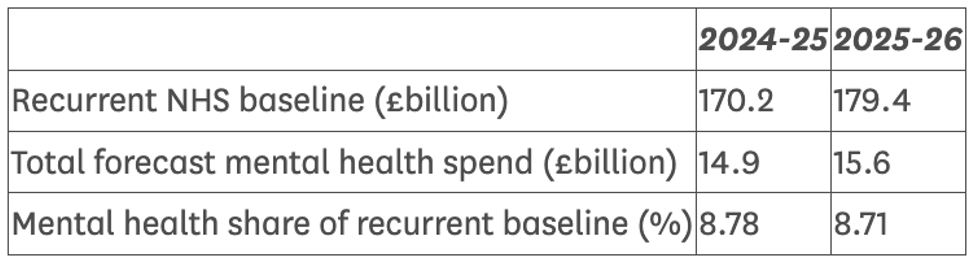
3) The government has announced a cut in the proportion of spending on mental health. This is on top of years of proportionately lower spending on mental health.
Mental Health: Expected Spend for 2025-26 Statement on 27 March 2025
4) The government announced on 22 April 2025 that it intends to hold a statutory public inquiry into the mental health homicides and attempted murders in Nottingham, which will be chaired by a retired circuit judge, HH Deborah Taylor:
“Resident Judge at Southwark Crown Court and Recorder of Westminster until her retirement from the Judiciary in December 2022. In 2022 she was Treasurer of Inner Temple, where she advocated for greater diversity at the Bar.
Deborah will continue in her role as Chair of the Criminal Legal Aid Advisory Board which she has held since July 2023.”
The terms of reference for this statutory inquiry have not yet been published.

So shocking, disgusting, horrific what other adjectives suffice? . A scandal in plain sight. A conspiracy of negligence What has HSSIB to day? Demand to be done?All those voices ignored and so more lost. Permanently Ar the same time assisted suicide is rushed through. Sinister You can publish this and previous comment anonymously Richard
Yahoo Mail: Search, organise, conquer
LikeLike